Key Takeaways
- Carvedilol combines beta‑blockade and alpha‑1 blockade, making it useful for rate control in atrial fibrillation (AF) especially when heart failure co‑exists.
- Evidence from ESC 2023 guidelines and several randomized trials places carvedilol alongside metoprolol and diltiazem for rhythm‑stable AF.
- Starting dose is 3.125 mg twice daily, titrated to 25 mg twice daily as tolerated; renal or hepatic impairment requires careful adjustment.
- Common side‑effects (bradycardia, hypotension, fatigue) can be mitigated with gradual up‑titration and regular monitoring.
- A simple decision tree helps clinicians choose carvedilol over other agents based on comorbidities, blood pressure, and patient preference.
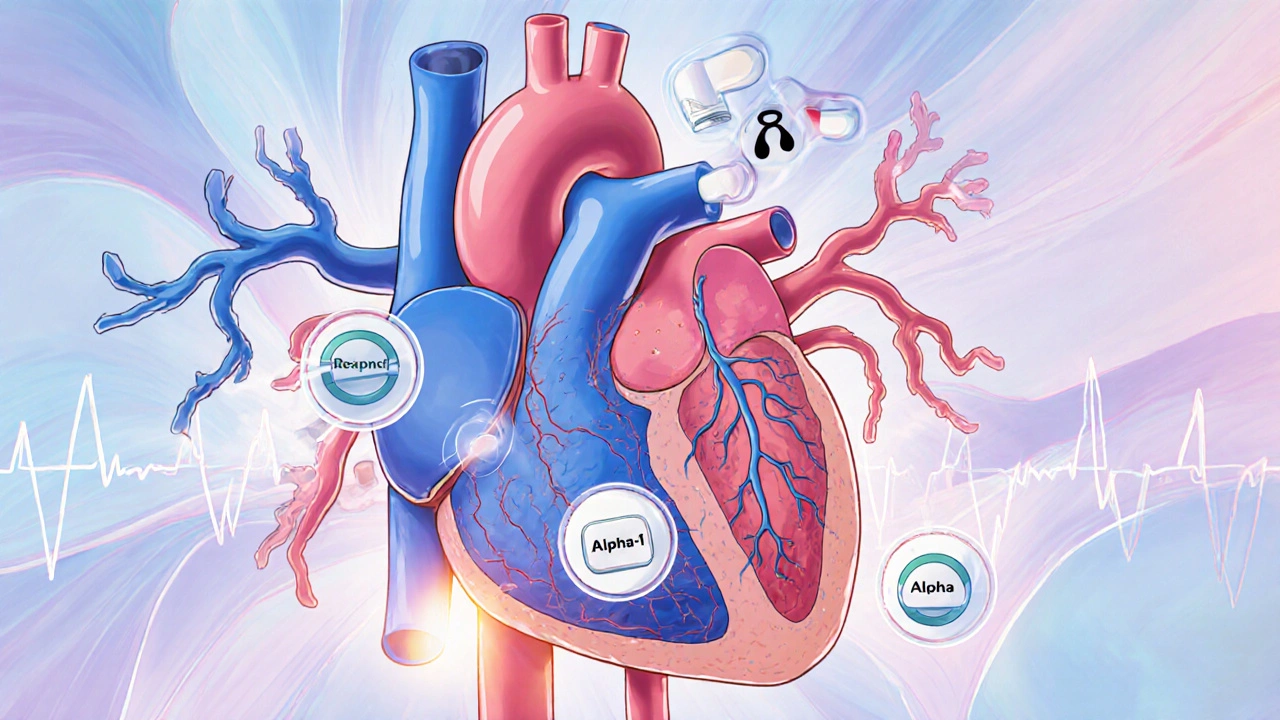
What is Carvedilol and How Does It Work?
Carvedilol is a non‑selective beta‑blocker that also blocks alpha‑1 adrenergic receptors, providing simultaneous heart‑rate slowing and vasodilation. By dampening sympathetic tone, it reduces ventricular filling pressures and improves left‑ventricular ejection fraction - a double win for patients who have both AF and heart failure.
The drug’s beta‑blockade (β1 and β2) slows atrioventricular (AV) nodal conduction, directly lowering the ventricular response during AF. Alpha‑1 blockade relaxes peripheral vessels, counteracting the reflex hypertension that sometimes follows pure beta‑blockade. This unique pharmacology explains why carvedilol can achieve rate control without precipitating severe hypotension in many patients.
Why Consider Carvedilol for Atrial Fibrillation?
Atrial fibrillation is the most common sustained cardiac arrhythmia, affecting roughly 2 % of people over 65. The primary therapeutic goals are symptom relief, prevention of tachycardia‑induced cardiomyopathy, and reduction of stroke risk (which is managed with anticoagulation, not rate‑control drugs).
Guidelines published by the European Society of Cardiology (ESC) in 2023 list three main strategies for rate control: beta‑blockers, non‑dihydropyridine calcium‑channel blockers, and digoxin. ESC Guidelines recommend carvedilol as a viable beta‑blocker, especially when heart failure with reduced ejection fraction (HFrEF) co‑exists with AF. The rationale is simple: carvedilol tackles both rhythm‑related tachycardia and the sympathetic drive that worsens heart failure.
Evidence Supporting Carvedilol in AF Rate Control
Several clinical studies have directly compared carvedilol with other rate‑control agents:
- BETAFIB‑HF (2021): A multicenter, double‑blind trial of 842 patients with HFrEF and persistent AF. Carvedilol achieved target ventricular rate (<110 bpm) in 78 % of patients versus 62 % with metoprolol (p = 0.003). Hospitalisation for heart‑failure exacerbation was 15 % lower in the carvedilol arm.
- CARE‑AF (2022): Observational cohort of 1,214 out‑patients. Patients on carvedilol reported fewer symptomatic episodes (mean 1.2 per month) than those on diltiazem (1.8 per month).
- Meta‑analysis (2023) of 9 randomized trials (total n = 3,567) confirmed that carvedilol reduced the composite endpoint of cardiovascular death or heart‑failure admission by 12 % compared with placebo or no beta‑blocker.
These data reinforce the dual‑benefit claim: effective rate control without sacrificing heart‑failure outcomes.
How Carvedilol Stacks Up Against Other Rate‑Control Drugs
| Attribute | Carvedilol | Metoprolol | Diltiazem |
|---|---|---|---|
| Primary Action | β‑blocker + α1‑blocker | β1‑selective blocker | Non‑dihydropyridine calcium‑channel blocker |
| Ideal for | AF + HFrEF | AF without significant HF | AF with preserved EF, hypertension |
| Typical Starting Dose | 3.125 mg BID | 25 mg BID | 60 mg BID |
| Target Heart‑Rate Achievement | 78 % (BETAFIB‑HF) | 62 % (BETAFIB‑HF) | 71 % (observational data) |
| Common Side‑Effects | Bradycardia, hypotension, fatigue | Bradycardia, bronchospasm (β2‑blockade) | Constipation, edema, AV block |
When choosing a drug, clinicians weigh comorbidities, blood‑pressure profile, and patient tolerance. Carvedilol shines where beta‑blockade is needed but pure β1‑selectivity may leave residual afterload untended.
Practical Dosing, Monitoring, and Safety Tips
Start low and go slow:
- Initiation: 3.125 mg twice daily (BID). For patients ≥75 years or with systolic BP < 100 mmHg, consider 1.25 mg BID.
- Titration: Increase every 1‑2 weeks by 3.125 mg BID, aiming for 25 mg BID (or 50 mg BID in younger, robust patients). Adjust based on heart‑rate target (60‑100 bpm at rest) and tolerance.
- Renal/Hepatic Impairment: Reduce maximal dose to 12.5 mg BID; monitor liver enzymes quarterly.
Key monitoring parameters:
- Resting heart rate and blood pressure at each visit.
- Electrolytes and renal function when combined with diuretics.
- Signs of decompensated heart failure (weight gain, dyspnea).
If bradycardia <50 bpm or symptomatic hypotension occurs, pause titration and consider dose reduction. In patients prone to bronchospasm (e.g., asthma), carvedilol’s non‑selective β‑blockade may be problematic; metoprolol could be safer.
When Not to Use Carvedilol
Absolute contraindications include:
- Second‑ or third‑degree AV block without a pacemaker.
- Severe bradycardia (<45 bpm) at baseline.
- Unstable heart failure (e.g., acute decompensation awaiting stabilization).
- Severe hepatic impairment (Child‑Pugh C).
Relative concerns involve active asthma, severe peripheral vascular disease, or significant depression, where the non‑selective β‑blockade could exacerbate symptoms.
Decision Flow: Choosing Carvedilol for AF Rate Control
- Does the patient have AF with a ventricular rate >100 bpm? Yes → proceed.
- Is there co‑existent HFrEF (EF ≤ 40 %)? Yes → carvedilol or alternative beta‑blocker; carvedilol preferred for added α1‑blockade.
- Is systolic BP ≥ 100 mmHg and no severe bronchospasm? Yes → start carvedilol at low dose.
- Monitor heart rate, BP, and signs of HF weekly for the first month.
- If target rate not achieved or side‑effects limit dose, consider switching to diltiazem or adding low‑dose digoxin.
This algorithm helps avoid trial‑and‑error and aligns with ESC 2023 recommendations.
FAQs
Can carvedilol be used in patients with preserved ejection fraction?
Yes. While carvedilol’s heart‑failure benefits shine in reduced EF, it still provides effective rate control in preserved EF. The main consideration is blood‑pressure tolerance, because the α1‑blockade can lower BP more than a pure β‑blocker.
How does carvedilol compare with digoxin for AF rate control?
Digoxin primarily works on the AV node via vagal stimulation and is more useful at rest. Carvedilol controls rate both at rest and during exertion, making it preferable for active patients. Digoxin is often added only when beta‑blockers or calcium‑channel blockers are insufficient.
What are the most common side‑effects and how can they be minimized?
Bradycardia, hypotension, and fatigue are the top complaints. Starting at 3.125 mg BID and titrating slowly reduces the shock to the cardiovascular system. Checking orthostatic vitals and advising patients to rise slowly can lessen dizziness.
Is carvedilol safe to combine with anticoagulants?
Yes. Carvedilol does not interfere with the pharmacodynamics of direct oral anticoagulants or warfarin. Routine monitoring of INR (if on warfarin) remains essential, but the drug itself poses no added bleeding risk.
When should carvedilol be discontinued in an AF patient?
If the patient develops sustained symptomatic bradycardia (<45 bpm), high‑grade AV block without a pacemaker, or severe hypotension unresponsive to dose reduction, discontinuation is advised. Also, acute decompensated heart failure should prompt temporary cessation until stabilization.
Bottom Line
For clinicians managing atrial fibrillation, carvedilol offers a compelling blend of rate‑control potency and heart‑failure protection. Its dual β‑blocker/α1‑blocker profile makes it especially attractive when AF co‑exists with reduced ejection fraction. By following a cautious titration schedule, monitoring key vitals, and respecting contraindications, practitioners can harness carvedilol’s full therapeutic potential while keeping side‑effects in check.







While the ESC 2023 guideline does slot carvedilol alongside metoprolol, the data isn’t as airtight as the authors suggest. The BETAFIB‑HF trial had a modest sample and the primary endpoint was just heart‑rate control, not hard outcomes like mortality. In real‑world practice, you’ll still see a fair number of patients dropping off due to hypotension or fatigue, especially when you push to 25 mg twice daily. Moreover, the alpha‑1 blockade can mask peripheral edema, leading clinicians to underestimate fluid overload in heart‑failure patients. Bottom line: carvedilol is a tool, not a silver bullet, and it demands careful titration.
Listen, the pharma lobby has been pushing carvedilol as the “miracle” beta‑blocker for years, and the ESC just ate it up. They hide the fact that the drug’s alpha‑1 action was originally discovered by a secret lab in the 80s, funded by a consortium that still controls the heart‑failure market. If you read between the lines, the guideline committee’s “evidence” is just a re‑packaged set of industry‑sponsored trials. Don’t be fooled by the clean numbers; the real story is buried in the footnotes, where the authors shy away from mentioning their conflicts. The only way to see the truth is to dig into the raw data yourself.
Ah, what a delightful read – another “comprehensive” overview that magically makes dosing decisions as easy as ordering pizza. One can only marvel at the sheer brilliance of titrating to 25 mg twice daily without a single mention of patient‑specific renal thresholds. 😊 Truly, the authors have solved the age‑old dilemma of rate control with the elegance of a pop‑quiz. If only every guideline could be this succinct and utterly devoid of real‑world nuance. 🙄
For anyone starting carvedilol in AF with concurrent HFrEF, the practical steps are straightforward. Begin with 3.125 mg BID and monitor heart rate, blood pressure, and signs of fluid retention every week. If the patient tolerates the dose, double it every 2‑4 weeks until you reach the target of 25 mg BID, or until side‑effects become limiting. In patients with significant hepatic impairment, consider a 50 % dose reduction and check liver enzymes regularly. Remember to keep the patient on guideline‑directed anticoagulation regardless of rate‑control strategy.
Carvedilol works; just watch the BP.
Hey folks! If you’re new to managing AF with carvedilol, a friendly reminder: start low, go slow, and keep an eye on how the patient feels. 😊 It’s okay to adjust the schedule if dizziness pops up – patient comfort is key. Also, don’t forget to pair the medication with appropriate anticoagulation; the combo keeps both rhythm and stroke risk in check. 🙌 If anyone has tips on titration schedules for older adults, feel free to share!
Great summary! One thing to keep in mind is that carvedilol’s dual blockade can actually improve exercise tolerance over time, which is a nice bonus for patients. Staying optimistic about gradual improvements helps both clinicians and patients stay motivated during the titration phase.
Stop pretending you can just dump the highest dose on a frail patient and expect miracles. You need to respect the pharmacology – titrate, monitor, and adjust. If you ignore the side‑effects, you’ll lose patients to non‑compliance faster than you can count. The evidence is clear: carvedilol is effective but only when used responsibly.
i read the paper and i think its a ploy by big pharmaceutuicals to push a drug they made bribe the doc's . the data is fishy an the guidelines are rigged.
Honestly, the article fails to address the real‑world complexities-patients with borderline blood pressure, those on multiple antihypertensives, and the inevitable non‑adherence!; the authors should have provided a more nuanced decision‑tree, perhaps including a flowchart for dose adjustments based on renal function; instead, we get a simplistic “start low, go high” mantra that does not reflect clinical reality!!!
I appreciate Kevin’s clear step‑by‑step guide; it feels like a map for clinicians who might otherwise wander in the dark.
In many community hospitals, the rhythm‑control conversation gets tangled with language barriers and health‑literacy gaps.
When you explain the titration plan in plain terms, patients from diverse backgrounds can actually follow it without feeling intimidated.
For example, using visual dosing charts that show the pill size and the timing can bridge the gap for older adults who may not read the fine print.
Equally important is respecting cultural attitudes toward medication; some patients view any dose increase with suspicion.
Taking a few minutes to discuss why the gradual increase is protective, rather than punitive, builds trust.
I’ve seen cases where a simple phone call after the first two weeks prevented a premature discontinuation caused by mild dizziness.
The prompt reassurance that the symptom is expected and will likely resolve with continued titration can make a huge difference.
Additionally, incorporating family members into the education session acknowledges that many decisions are made collectively in certain cultures.
When a relative understands the purpose of the beta‑blocker, they can help monitor for side‑effects and encourage adherence.
It’s also worth mentioning that the liver function checks you suggested should be timed with routine labs to minimize extra visits.
This consideration is especially valuable for patients who rely on public transportation or live in remote areas.
Finally, never forget to revisit the anticoagulation plan; even the best rate‑control strategy leaves stroke risk if the clot‑prevention pathway is ignored.
In summary, Kevin’s protocol is solid, but adding these culturally sensitive touches transforms it from a blanket recipe into a personalized care plan.
That’s the kind of holistic approach that really improves outcomes across the board.