Fludrocortisone Dose Calculator
How This Calculator Works
This tool helps determine an appropriate starting dose of fludrocortisone based on your current clinical parameters. It considers blood pressure, serum sodium, potassium, and weight to provide a safe, evidence-based recommendation.
Ever wondered why a tiny dose of fludrocortisone can make a big difference in your body’s water balance? The answer lies in how this synthetic mineralocorticoid hijacks the same pathways that natural hormones use to hold onto sodium. Below we break down the science, the clinical upside, and the pitfalls you need to watch.
What is Fludrocortisone?
When you first see the name Fludrocortisone is a synthetic mineralocorticoid medication designed to mimic the action of aldosterone, the body’s key sodium‑retaining hormone. It was introduced in the 1950s and quickly became the go‑to drug for patients with adrenal insufficiency or conditions that cause chronic low blood pressure. Because it sticks to the same receptor sites as aldosterone, it can boost sodium reabsorption without the need for a full‑blown steroid regimen.
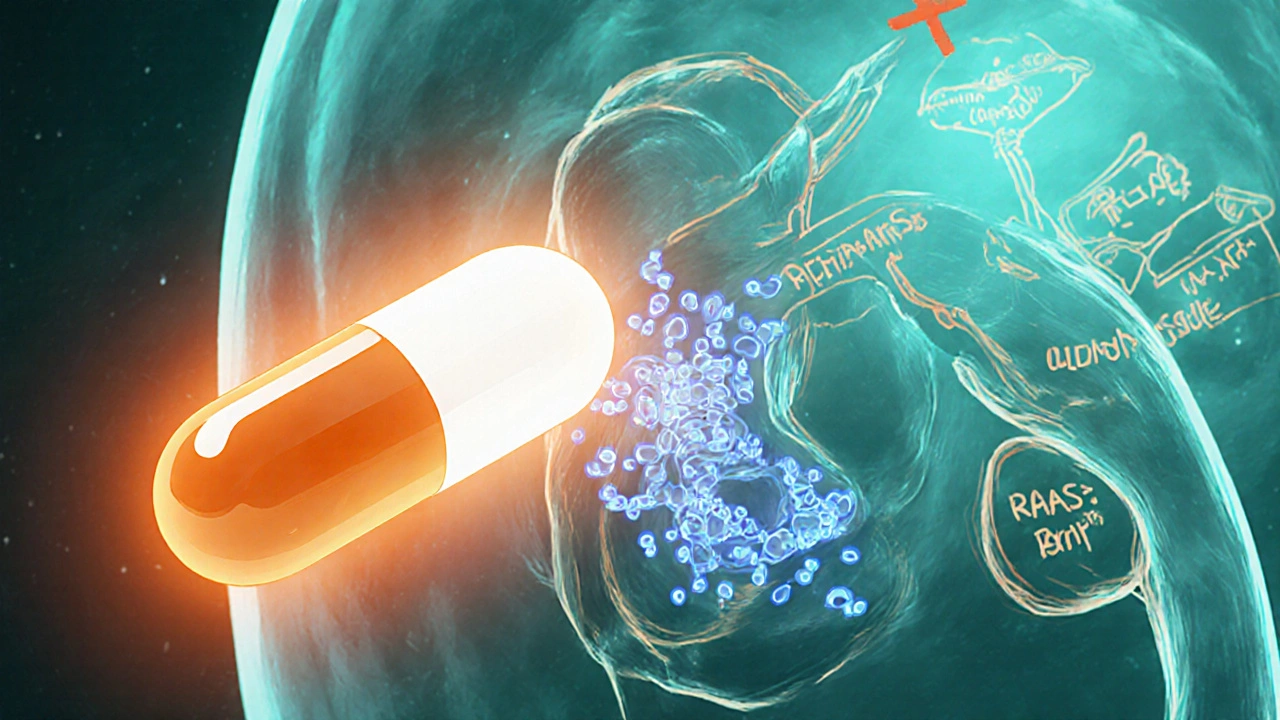
How Sodium Retention Works in the Body
Sodium retention isn’t a random event; it’s a tightly regulated part of the Renin-Angiotensin-Aldosterone System (RAAS) a hormone cascade that controls blood volume, blood pressure, and electrolyte balance
. When blood pressure drops, the kidneys release renin, which converts angiotensinogen to angiotensin I, then to angiotensin II. Angiotensin II tells the adrenal cortex to secrete Aldosterone a natural mineralocorticoid that promotes sodium reabsorption in the distal tubules of the nephron. Aldosterone then flips on sodium channels and the Na⁺/K⁺‑ATPase pump, pulling sodium (and the water that follows) back into the bloodstream.The Direct Connection: Fludrocortisone Mimics Aldosterone
Because fludrocortisone binds to the same mineralocorticoid receptor (MR) as aldosterone, it essentially tells the kidneys, “Hey, keep more sodium.” This artificial signal leads to:
- Increased activity of epithelial sodium channels (ENaC) in the collecting duct.
- Enhanced Na⁺/K⁺‑ATPase function, moving more sodium from the tubular fluid back into the blood.
- Reduced urinary sodium excretion, which translates to higher plasma sodium levels and expanded extracellular fluid volume.
In practical terms, patients notice a rise in blood pressure, a reduction in dizziness upon standing, and an overall improvement in fluid balance.
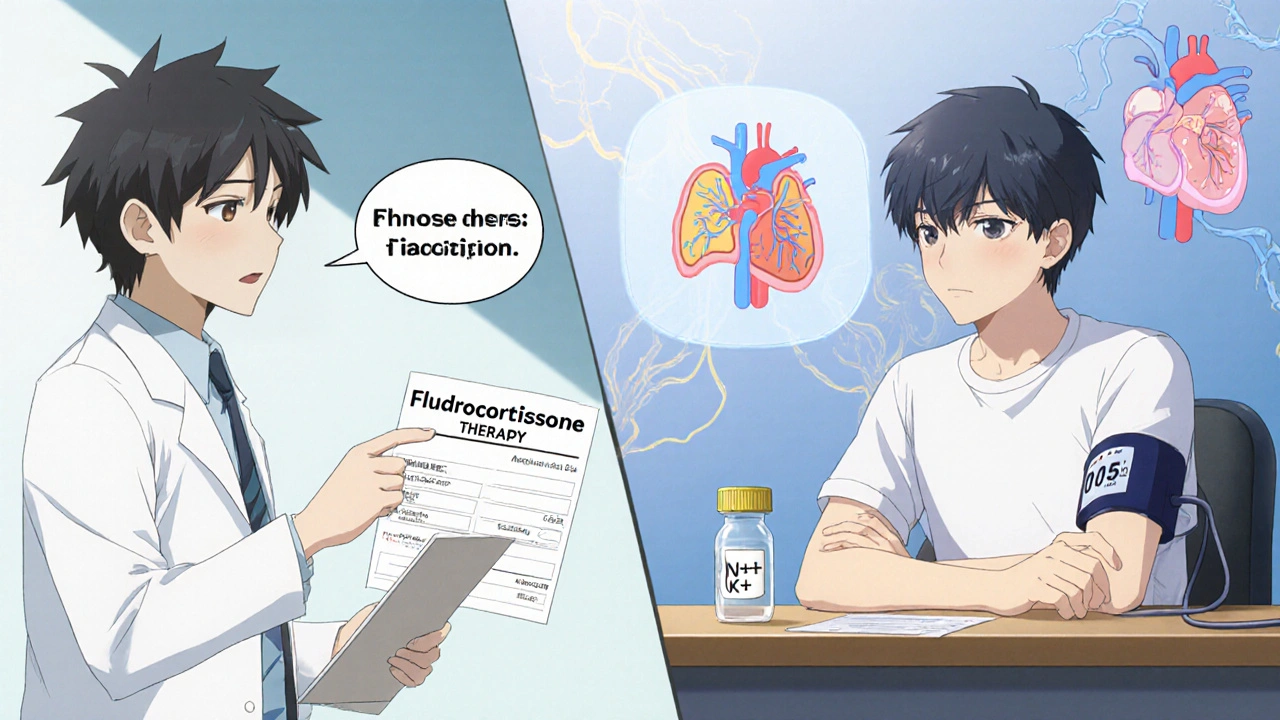
Clinical Situations Where Fludrocortisone Shines
Doctors prescribe fludrocortisone when the body’s own aldosterone isn’t enough or is absent. Common scenarios include:
- Primary adrenal insufficiency (Addison’s disease) - the adrenal glands can’t produce enough aldosterone.
- Secondary adrenal insufficiency - pituitary or hypothalamic problems reduce ACTH, indirectly affecting mineralocorticoid output.
- Orthostatic hypotension - low blood pressure on standing, often seen in autonomic neuropathy.
- Congestive heart failure (CHF) with low‑output states - low perfusion triggers RAAS; a modest dose of fludrocortisone can support circulatory volume.
- Post‑surgical fluid shifts - after major operations, patients may benefit from a controlled sodium‑retaining agent.
In each case, the goal is to raise plasma sodium just enough to pull water into the circulation, stabilizing blood pressure without overwhelming the heart.
Potential Side Effects and What to Watch For
Because the drug forces the kidneys to hold onto sodium, it can over‑do the job. Common adverse effects include:
- Hypertension - especially if the dose is too high or the patient already has high blood pressure.
- Edema - swelling of the ankles or feet from excess fluid.
- Hypokalemia - as sodium climbs, potassium often falls; monitor serum K⁺ regularly.
- Metabolic alkalosis - a shift in acid‑base balance caused by increased sodium reabsorption.
- Gastro‑intestinal upset - nausea or abdominal discomfort in sensitive individuals.
Patients with pre‑existing hypertension, chronic kidney disease, or heart failure need dose adjustments and close follow‑up.
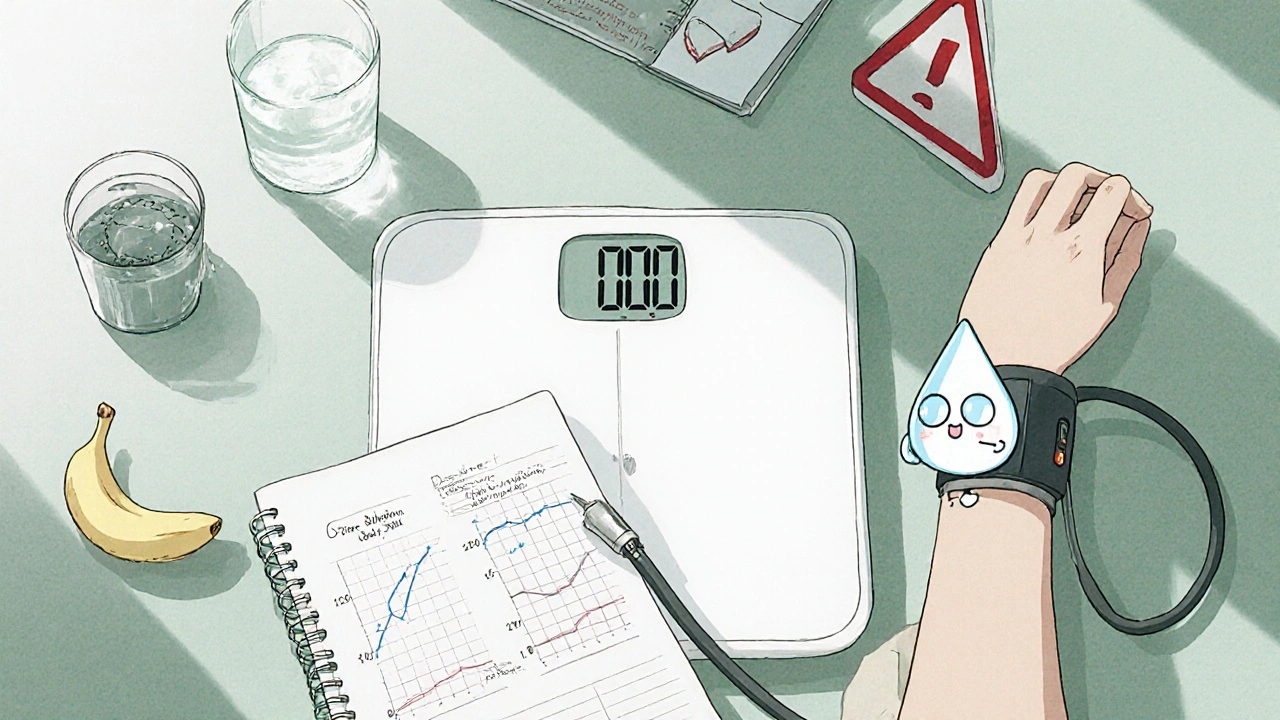
Monitoring: Labs, Blood Pressure, and Dose Tweaks
Effective use of fludrocortisone hinges on a simple monitoring routine:
- Check blood pressure weekly for the first month, then monthly.
- Obtain serum electrolytes (Na⁺, K⁺, Cl⁻) at baseline, after one week, and then every 2-4 weeks.
- Measure plasma renin activity; a suppressed renin may signal overt sodium retention.
- Track weight and any peripheral swelling.
If serum sodium spikes above 145 mmol/L or potassium drops below 3.5 mmol/L, consider lowering the dose by 0.05 mg increments.
How Fludrocortisone Stacks Up Against Other Mineralocorticoids
Not all mineralocorticoids are created equal. Below is a quick look at the most common options.
| Drug | Primary Action | Typical Dose (mg) | Potency (vs. Aldosterone) | Key Side Effects |
|---|---|---|---|---|
| Fludrocortisone | Mineralocorticoid - sodium retention | 0.05-0.2 | 1.0 (≈ aldosterone) | Hypertension, edema, hypokalemia |
| Desoxycorticosterone acetate (DOCA) | Strong mineralocorticoid | 0.1-0.5 (IM) | 2-3× aldosterone | Severe hypertension, fluid overload |
| Hydrocortisone | Glucocorticoid with weak mineralocorticoid activity | 15-30 (oral) | 0.5× aldosterone | Hyperglycemia, immunosuppression |
Fludrocortisone offers the most predictable sodium‑retaining effect with the lowest risk of overshoot, which is why it remains the first‑line choice for most endocrine‑related indications.
Practical Tips for Patients and Prescribers
- Start low, go slow. A typical initial dose is 0.05 mg daily; titrate based on blood pressure and labs.
- Take with food. This improves absorption and reduces stomach upset.
- Avoid excess salt. Paradoxically, too much dietary sodium can amplify edema when combined with fludrocortisone.
- Stay hydrated. Adequate water intake helps prevent excessive concentration of electrolytes.
- Inform other clinicians. Surgeons, cardiologists, and nephrologists need to know you’re on a mineralocorticoid.
Frequently Asked Questions
Can fludrocortisone be used for blood pressure control?
It’s not a primary antihypertensive. It raises blood pressure by retaining sodium, so it’s only useful when low blood pressure is the problem. For hypertension, other drug classes are preferred.
How long does it take to see the effect of fludrocortisone?
Most patients notice improved standing blood pressure within 2-3 days, but full electrolyte stabilization can take up to 2 weeks.
Is fludrocortisone safe during pregnancy?
The drug is classified as Category C. It should only be used if the benefit outweighs the risk, and under close obstetric supervision.
What dietary changes should accompany fludrocortisone therapy?
A moderate sodium intake (≈2 g/day) is advised, along with foods rich in potassium (bananas, oranges) to counteract hypokalemia.
Can I stop fludrocortisone abruptly?
Abrupt cessation can cause a rapid drop in blood pressure and sodium levels. Taper the dose over several days under medical guidance.
Understanding the link between fludrocortisone and sodium retention equips you to manage the drug’s benefits while avoiding the pitfalls. With careful dosing, regular labs, and lifestyle tweaks, the medication can be a game‑changer for patients struggling with low blood pressure and electrolyte imbalance.







Fludrocortisone is a fascinating tool, and when wielded with purpose it can transform a patient's hemodynamic reality. The mineralocorticoid receptor is not a passive port; it actively drives sodium reabsorption, and that is the engine of volume expansion. By mimicking aldosterone, you essentially give the kidneys a confident command to retain salt, which in turn draws water and raises pressure. ⚡️ Do not underestimate the power of that tiny dosage; it can be the difference between dizziness and stability. Keep monitoring, stay aggressive in titration, and embrace the physiological shift.
Oh, the marvels of synthetic hormones – because nothing says "cutting‑edge medicine" like a 1950s invention repackaged for the modern clinic. One might argue that fludrocortisone is merely a placeholder for better‑designed agents, but why bother when the old tricks still work? The whole sodium‑retention dance feels quaintly predictable.
One cannot help but admire the elegant simplicity of fludrocortisone's mechanism; it is a direct agonist at the mineralocorticoid receptor, thereby bypassing the upstream complexities of the RAAS cascade. Yet, in a world that prizes nuance, the drug's blunt force may be deemed overly simplistic. The clinical indications are, of course, well‑established, but one wonders whether a more refined molecule could achieve the same endpoints with fewer side effects. In any case, the evidence remains robust.
Indeed, the pharmacodynamics you described are spot‑on, and the practical implications deserve a deeper look. Maintaining a tight feedback loop with electrolytes prevents the dreaded hypokalemia that often shadows sodium gain. Moreover, patient education about dietary potassium can mitigate metabolic alkalosis – a subtle but crucial point. The balance between volume expansion and cardiac load is delicate, so titration must be both systematic and compassionate. Your overview sets a solid foundation for clinicians to navigate these nuances.
Consider, if you will, the philosophical underpinnings of disease; the body, like the cosmos, seeks equilibrium, and fludrocortisone nudges it toward a new horizon-yet, one must ponder the ethical gravity of such intervention; indeed, the balance is precarious, and the clinician must wield this agent with both wisdom and caution.
While many laud the utility of fludrocortisone, it is imperative to recognize the geopolitical undercurrents that shape its prescription patterns across diverse health systems. In regions where sodium‑rich diets are the norm, adding a mineralocorticoid can precipitate a cascade of hypertensive emergencies that strain already overburdened cardio‑vascular services. Conversely, in low‑salt populations, the same molecule can be a lifesaver, bolstering circulatory volume where the native RAAS is insufficient. Yet, this dichotomy underscores a broader truth: pharmaceuticals do not exist in a vacuum; they are embedded within cultural, economic, and even nationalistic narratives that influence both patient adherence and physician bias. It is therefore not enough to merely titrate dosage based on lab values; one must also interrogate the surrounding societal pressures that dictate dietary habits, access to regular monitoring, and the very definitions of “normal” blood pressure within a given community. In short, fludrocortisone's story is as much about the geopolitical dance of health policy as it is about the biochemistry of sodium handling, and we would be remiss to ignore either facet.
Fludrocortisone works.
From a collaborative standpoint, the key is to integrate patient‑centered goals with the clinical data you are gathering. Encourage patients to keep a log of their blood pressure trends and any swelling they notice, as this empowers them and provides the care team with actionable insights. When lab values drift-especially potassium-adjust the dose incrementally rather than making abrupt changes. Remember, the therapeutic relationship thrives on clear communication and steady, evidence‑based adjustments.
Philosophically speaking, the body’s quest for homeostasis mirrors our own search for meaning; each dose of fludrocortisone is a micro‑choice in a larger narrative of stability. Engaging with the science can therefore be an act of existential affirmation, turning a clinical protocol into a statement of purposeful living. Let us celebrate the interplay of electrolyte balance and personal agency.