Warfarin Binge Risk Calculator
Calculate Your Risk
What This Means
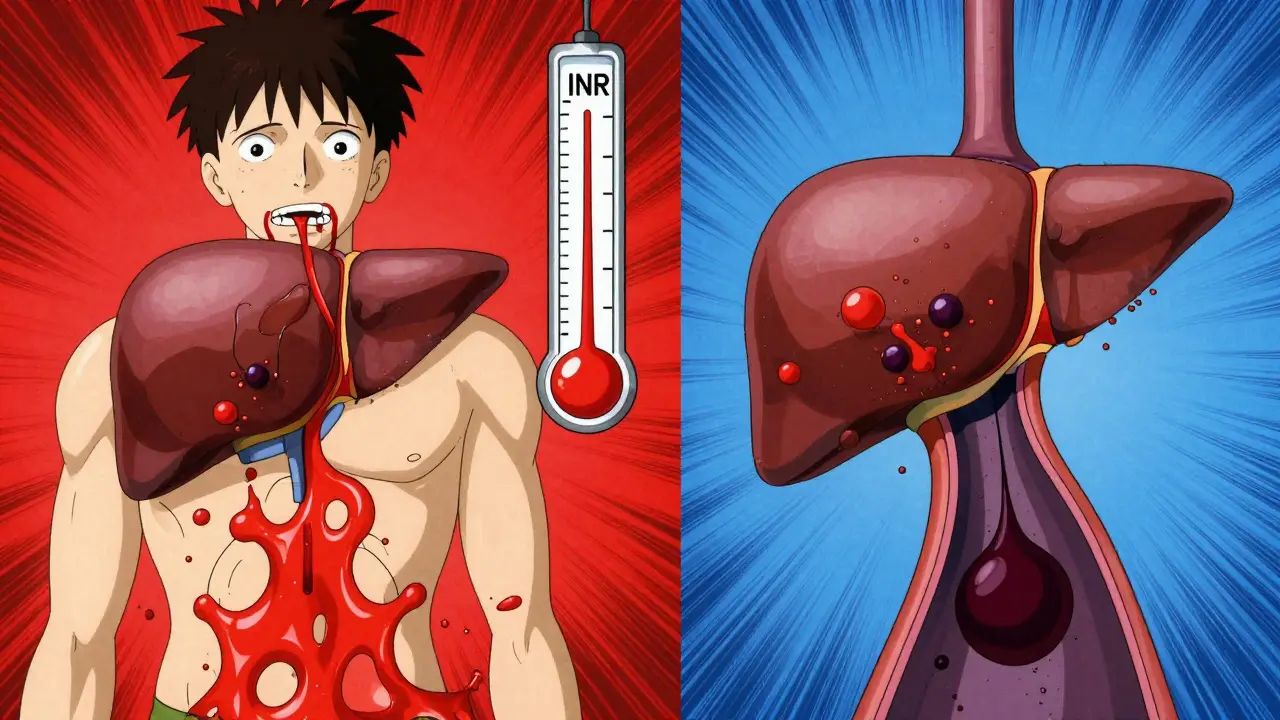
If you're taking warfarin, drinking too much alcohol in one sitting isn't just a bad idea-it can be life-threatening. Warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, deep vein thrombosis, or after a pulmonary embolism, works by blocking vitamin K. But its effect is delicate. Too little, and you risk a clot. Too much, and you bleed. The narrow window between safety and danger is called the therapeutic range: an INR between 2.0 and 3.0. Now, add binge drinking to that equation, and everything becomes unpredictable.
What Counts as Binge Drinking?
The National Institute on Alcohol Abuse and Alcoholism defines binge drinking as consuming five or more drinks in about two hours for men, or four or more for women. That’s not a night out-it’s a spike in alcohol that hits your liver hard. One drink means 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of hard liquor. Five drinks in two hours? That’s a six-pack of beer or five shots of whiskey in a short time. For someone on warfarin, this isn’t about getting drunk-it’s about triggering a dangerous chemical chain reaction in your body.
How Alcohol Throws Your INR Off Balance
Your liver doesn’t just process alcohol-it also breaks down warfarin. The same enzymes, CYP2C9 and CYP3A4, handle both. When you binge drink, your liver gets overwhelmed. At first, alcohol blocks warfarin from being broken down. That means more warfarin stays in your blood, your INR spikes, and your risk of bleeding skyrockets. This can happen within hours. You might feel fine, but your blood is thinning faster than your doctor expects.
Then comes the second phase. If you binge regularly, your liver adapts. It starts producing more of those enzymes. Now it breaks down warfarin too fast. Your INR drops. Your clotting risk goes up. You’re stuck in a cycle: one binge raises your INR, the next lowers it. Your doctor can’t keep up. Routine INR checks every four weeks? That’s not enough. A single binge can send your INR into the danger zone between visits.
A 2015 study from the University of Michigan tracked over 1,200 patients on warfarin. Those who binged alcohol had more than double the risk of major bleeding-like internal bleeding, brain hemorrhages, or uncontrollable nosebleeds. For people on warfarin for over a year? The risk jumped to over three times higher. Why? Because long-term alcohol use damages the liver, making it worse at producing clotting factors. Even if your warfarin dose is perfect, your body’s ability to control bleeding is crumbling.
Genetics Make It Worse
Some people have a genetic quirk that makes this even more dangerous. About 10% of people carry variants called CYP2C9*2 or CYP2C9*3. These versions of the enzyme break down warfarin much slower. If you have one of these, your body already holds onto warfarin longer. Add alcohol, and your INR can shoot up 40-50% higher than someone without the variant. The same Michigan study found these patients had a 4.2-fold higher risk of major bleeding after binge drinking. This isn’t rare-it’s a hidden risk many doctors don’t test for.
What the Experts Say
The British Heart Foundation says it plainly: "It’s OK to drink alcohol if you’re on warfarin, but never all 14 units in one week-and never in one day." That’s about six pints of beer or six glasses of wine. The NHS warns: "Drinking heavily, especially binge drinking lots of alcohol in one go, is dangerous while taking warfarin. The alcohol can increase the risk of bleeding." The American Heart Association and European Society of Cardiology both recommend limiting alcohol to no more than 8-10 units per week. That’s roughly one drink a day, max. But here’s the catch: even one drink can cause a swing in INR. A 2020 analysis of over 12,000 patients showed that those who binged at all spent 42% more time outside the safe INR range than those who didn’t drink. That’s not a small difference-it’s a medical emergency waiting to happen.
Warning Signs You’re Bleeding
When your INR spikes because of alcohol, you might not notice until it’s too late. Bleeding doesn’t always come with a scream. Look for these signs:
- Unusual bruising, especially large purple patches without injury
- Nosebleeds that won’t stop
- Bleeding gums when brushing your teeth
- Bright red blood in stool or black, tar-like poop
- Brown or red urine
- Coughing up blood or bloody mucus
- Severe headaches, dizziness, or weakness
- Excessive menstrual bleeding
- Sharp abdominal pain or vomiting that looks like coffee grounds
If any of these happen, call your doctor or go to the ER. Don’t wait. A bleed in the brain or gut can kill you within hours.
What About Other Blood Thinners?
You might think switching to a newer drug like rivaroxaban or apixaban solves the problem. It doesn’t. The FDA’s own adverse event database shows heavy drinkers on these drugs have an 1.8-fold higher risk of stomach bleeding. Alcohol doesn’t just interfere with warfarin-it’s risky with all anticoagulants. The difference? Warfarin has a clear warning sign: your INR. With newer drugs, you don’t get that feedback. You’re flying blind.

What Should You Do?
If you’re on warfarin and drink, here’s what you need to do:
- Never binge. Even one binge episode can be dangerous.
- Stick to one drink per day at most. Two drinks on special occasions? Maybe-but not often.
- Get your INR checked within 72 hours after any alcohol use. Routine monthly checks aren’t enough.
- Tell your anticoagulation clinic or pharmacist if you drink. They need to know.
- If you can’t cut back, talk to your doctor about switching to a different anticoagulant-or getting help for alcohol use.
There’s hope. A 2022 study called the WAVE trial showed that patients who got regular counseling about alcohol and warfarin had 37% fewer bleeding events. Simple conversations-repeated over time-work. Your doctor can’t help if you don’t tell them the truth.
When to Consider a Change
The UK’s NICE guidelines say this clearly: if you regularly drink more than the recommended limits, you should be offered a different anticoagulant. DOACs like apixaban or dabigatran don’t need INR checks. They’re easier to manage. But they’re not safer with alcohol. They just hide the danger. If you can’t control your drinking, the best option might be to stop alcohol entirely-and get help doing it.
Integrated care programs-where addiction specialists work with anticoagulation clinics-have cut major bleeding by over half in patients with alcohol use disorder. That’s not a miracle. It’s science. If you’re struggling, ask for help. Your life depends on it.
Final Warning
Warfarin isn’t just a pill. It’s a balancing act. Alcohol doesn’t just interfere with it-it turns the balance into a seesaw. One binge can send you into the ER. Repeated binges can kill you quietly, over time. The data is clear. The guidelines are loud. The risk isn’t theoretical. It’s real. And it’s happening every day.
You don’t need to quit alcohol forever. But you do need to stop drinking it in large amounts. One drink, occasionally, is manageable. Five drinks in one night? That’s not a celebration. It’s a gamble with your life.








So I just got back from my doc’s office after my INR came back at 4.8… and yeah, I had that one night where I did 6 beers. Not cool. I thought I was fine since I don’t drink often. Turns out, even one binge is like tossing a match into a gas can. 😅
Alcohol + warfarin = a masterclass in self-sabotage. The liver isn’t some magical detox machine-it’s a stressed-out intern working double shifts. Binge drinking doesn’t just ‘throw off’ your INR-it throws the whole damn system into chaos. And people wonder why they end up in the ER with a brain bleed. 🤦♂️
It is imperative to underscore, with unequivocal clarity, that the consumption of alcohol-particularly in excessive, episodic quantities-is not merely inadvisable, but fundamentally incompatible with the physiological stability required for safe anticoagulation therapy. The data are not ambiguous. The risks are not hypothetical. The consequences are irreversible.
I’ve been on warfarin for 7 years, and honestly? I stopped drinking entirely after I saw a friend lose a kidney to a bleed. It’s not about being perfect-it’s about being alive. One drink on my birthday? Fine. But I don’t do ‘binges.’ I do ‘living.’ And I’m still here. 💪
Look, I get it. You think you’re just having a good time. But this ain’t Europe. This is America. We don’t gamble with our lives. If you’re on warfarin and you’re bingeing, you’re not just risking your own life-you’re wasting hospital beds, clogging up the system, and making it harder for people who actually need care. Stop being selfish.
One drink. That’s it.
I’m a clinical pharmacist, and I see this every single week. Patients think, ‘I had one night, it’s fine.’ Then their INR spikes, they get admitted, and they’re confused why. The liver doesn’t care if it’s Friday or Tuesday. It’s just doing its job-until it can’t. Please, if you drink, log it. Tell your anticoagulation team. They’re not judging. They’re saving your life.
So let me get this straight… you’re telling me that if I have a few shots on a Saturday night, my body might start bleeding internally… and I won’t even know until I’m coughing up blood? That’s not a medical condition-that’s a horror movie plot. And the scariest part? The newer drugs don’t even tell you it’s happening. I’m switching to aspirin. At least I know when I’m bleeding from that. 😅
Just wanted to say thank you for this. I’ve been on warfarin for 5 years and drank too much last year. I didn’t know the risk was this real. I’ve cut back to one drink once a month. My INR’s been stable since. You’re not alone. We can do this. 🙌
In India, many people think alcohol is safe if you drink slowly. But warfarin doesn’t care how fast you drink. Even small amounts every day can build up. Better to avoid it completely. Simple.
my doc told me to limit to 2 drinks a week but i still do 3 on weekends… i know i should stop but its hard. like… why does it have to be this complicated? 🤷♂️
Let’s be real here-this isn’t just about warfarin. This is about the broader epidemic of self-destruction disguised as ‘relaxation.’ The fact that people think a six-pack is a ‘social activity’ while on a life-saving medication speaks volumes about our cultural priorities. We glorify excess while ignoring consequence. And then we wonder why healthcare costs are astronomical. It’s not the system’s fault. It’s ours. And until we stop treating our bodies like disposable containers… we’ll keep ending up in trauma bays. The science is clear. The choice? Not so much.
Wait… so if I drink and my INR spikes, does that mean I’m literally one sip away from dying? Like… what if I just had one glass of wine? Is that a death sentence? I need to know. I need to know right now. I’m panicking. I just had one. Oh god. Oh god. Oh god.