When you fill a prescription for a generic pill-say, lisinopril for high blood pressure or metformin for diabetes-you probably assume it’s cheap because it’s generic. But why is it cheap? And who’s really making sure it stays that way? The truth is, the U.S. government doesn’t directly set prices for generic drugs like it does in Canada or the UK. Instead, it uses a mix of rebates, programs, and market rules to keep costs down. It’s not perfect, but it’s what’s keeping millions of Americans from paying hundreds of dollars a month for basic medicines.
How Medicaid Keeps Generic Prices Low
The biggest lever the federal government pulls to control generic drug prices is the Medicaid Drug Rebate Program. Since 1990, drugmakers have been required to give Medicaid a discount on every generic drug they sell. The rebate isn’t fixed-it’s calculated quarterly based on two numbers: the Average Manufacturer Price (AMP) and the Best Price the company offers any other buyer. The rebate is the higher of either 23.1% of AMP or the difference between AMP and that Best Price.
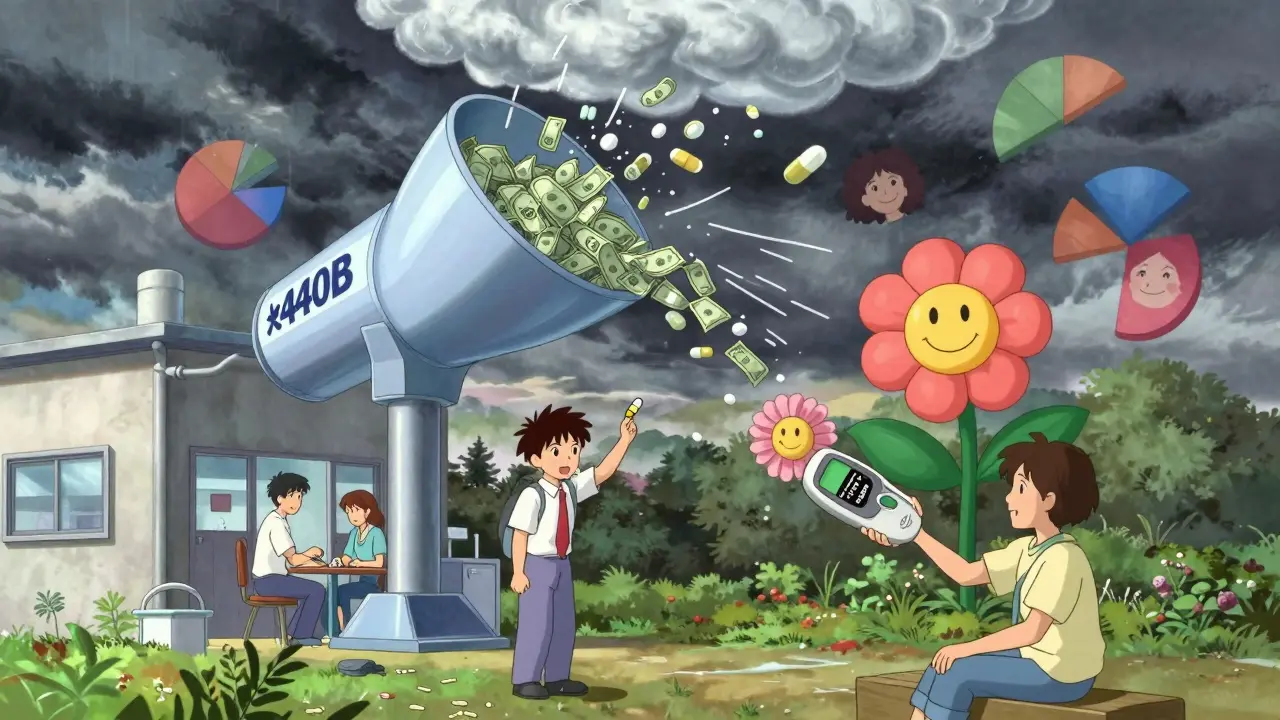
In 2024, this program brought in $14.3 billion in rebates from generic drugs alone-78% of all Medicaid drug rebates. That money doesn’t go to patients directly, but it lowers the overall cost of the program, which helps keep state and federal budgets from exploding. Without this system, many generic drugs would cost 30-50% more at the pharmacy counter.
Medicare Part D and the Out-of-Pocket Cap
If you’re on Medicare, your generic drug costs depend on your plan. In 2025, the standard Medicare Part D benefit requires you to pay 25% of the drug’s cost during the initial coverage phase. But here’s the big change: starting in 2025, the Inflation Reduction Act capped your total out-of-pocket spending on all drugs at $2,000 per year. That’s huge for people taking multiple generics.
Before the cap, some seniors paid over $400 a year just for their generic meds. Now, even if you take five or six generics, your annual cost is locked in. For low-income beneficiaries enrolled in the Low-Income Subsidy (LIS) program, the copay for generics is $0 to $4.90 per prescription-often less than the cost of a coffee. That’s not because the drug is free; it’s because the government pays the rest through rebates and subsidies.
The 340B Program: Discounted Drugs for the Poor
Another hidden engine of low generic prices is the 340B Drug Pricing Program. It forces manufacturers to sell outpatient drugs-both brand and generic-at deep discounts to hospitals and clinics that serve low-income patients. These aren’t charities; they’re safety-net providers like community health centers and rural hospitals.
On average, 340B discounts range from 20% to 50% below the regular manufacturer price. A 2025 survey by the Community Health Center Association found that 87% of these clinics reported better patient adherence because patients could finally afford their meds. One clinic in Mississippi saw diabetes medication use jump 40% after switching to 340B-priced generics. The program doesn’t touch your local pharmacy, but it keeps prices low for millions who rely on public health systems.
Why Generic Prices Still Spike
Here’s the catch: competition keeps prices low. But when there’s no competition, prices explode. In 2024, the generic drug pyrimethamine (Daraprim) jumped 300% in price after only two manufacturers remained in the market. The FDA approved dozens of generic versions over the years, but most companies stopped making it because the profit margin was too thin. When demand stayed steady and supply shrank, the remaining makers raised prices.
This isn’t rare. The same thing happened with doxycycline, nitrofurantoin, and even insulin generics. The market works fine when there are 10 or 15 makers. But if only one or two are left, they can play a game of chicken-and patients pay the price. The government doesn’t step in to force new manufacturers in. It just watches.
What’s Changing in 2026 and Beyond
The biggest shift coming is Medicare’s new ability to negotiate prices for certain high-cost drugs. But here’s the twist: most generics are excluded. The law says negotiation only applies to drugs with little or no competition. So if a generic has 5 or more makers, it’s off the table.
But there’s an exception. In 2027, CMS will negotiate prices for generic versions of apixaban (Eliquis) and rivaroxaban (Xarelto)-two blood thinners that had brand-name exclusivity until recently. Now that generics are flooding the market, why negotiate? Because these drugs are still expensive overall. With over 5 million Medicare patients using them, even a 30% price cut could save $1.2 billion over five years.
Some experts think this is a test run. If it works, the government may expand negotiation to other high-volume generics. Others say it’s too little, too late. The Congressional Budget Office estimates that extending negotiation to all generics could save $12.7 billion over ten years-but that’s only 0.3% of total drug spending. Still, it’s a start.
Why the U.S. Pays More Than Other Countries
Compared to other rich countries, the U.S. pays 1.3 times more for generic drugs on average. Why? Because other nations have centralized price setters. In the UK, NICE negotiates prices directly with manufacturers. In Germany, they require proof that a generic is worth its cost before allowing it on the market. In Canada, they cap prices based on what other countries pay.
The U.S. system relies on market competition. That’s great when there are 20 companies making a drug. It’s terrible when there are two. And because the U.S. doesn’t have a single buyer (like the NHS in the UK), there’s no leverage to push prices down. Private insurers, PBMs, and Medicare all buy separately, so no one has enough power to force a discount.

Who’s Really Making Money?
Here’s the dirty secret: most of the “savings” from generic drugs don’t reach patients. Pharmacy Benefit Managers (PBMs)-the middlemen between insurers, pharmacies, and drugmakers-collect rebates and negotiate discounts. But they don’t always pass those savings on.
A July 2025 Senate report found that 68% of generic drug rebates stay with PBMs. That’s why your copay might be $15 one month and $45 the next, even though your plan says the drug is “covered.” The pharmacy might have switched to a different generic version with a higher list price and a bigger rebate for the PBM. You don’t know. The pharmacist might not even know. The system is designed to hide the real cost.
What Works, What Doesn’t
What works: Medicaid rebates, the $2,000 out-of-pocket cap, 340B discounts, and rapid generic approvals by the FDA. These have kept 90% of U.S. prescriptions filled with generics.
What doesn’t: the lack of price transparency, the PBM rebate system, and the absence of any mechanism to prevent price gouging when competition disappears. The government lets the market run free-until it breaks. Then it does nothing.
Experts are split. The Academy of Managed Care Pharmacy says more competition is the answer-no price controls. Dr. Peter Bach says Medicare should act like the VA, which gets 40-60% discounts by buying in bulk. The industry warns that too much control will kill innovation. But innovation isn’t the problem here. It’s profit chasing in markets with no buyers.
What You Can Do
If you’re on Medicare, use the Medicare Plan Finder tool. Compare plans not just by premium, but by how much you’ll pay for your specific generics. Some plans have $0 copays for certain drugs. Others don’t.
Ask your pharmacist: “Is this the lowest-cost generic version?” Sometimes, switching brands cuts your cost by half.
Check if your clinic is a 340B provider. If you’re low-income, you might qualify for discounts even without insurance.
And if your bill jumps unexpectedly? Call your plan. Ask for a breakdown of the price change. You’re not being paranoid-you’re being smart.