Every year, millions of people in the U.S. take medications past their expiration date-not because they’re reckless, but because they don’t know what to do with them. You’ve probably got a drawer or cabinet full of old pills: that leftover antibiotic from last winter, the insulin pen you didn’t finish, the birth control pack you switched off. You don’t throw them out. You don’t know if they’re still safe. And you definitely don’t have a system to check them.
Here’s the truth: medication expiration dates aren’t just paperwork. They’re safety markers. Some drugs lose potency fast. Others stay stable for years. But without a simple, regular review process, you’re gambling with your health-and wasting money. The FDA estimates that improper medication use contributes to 125,000 deaths a year in the U.S. A lot of those are preventable. The fix isn’t complicated. It’s a schedule.
Why You Need a Medication Expiration Review Schedule
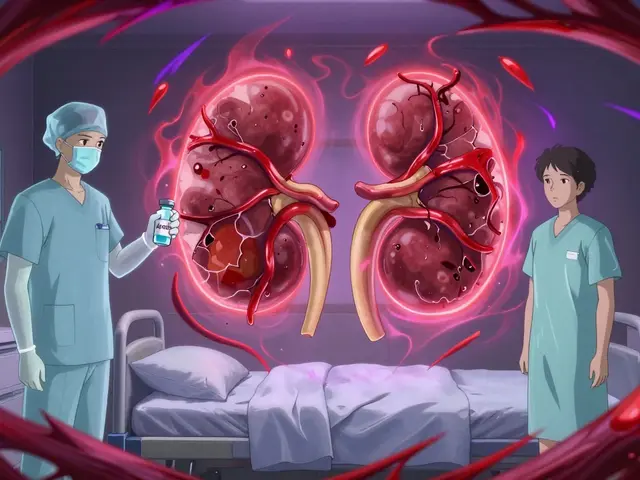
Expiration dates tell you when a drug is guaranteed to work as intended. That doesn’t mean it turns toxic the next day. But it does mean you can’t count on it. Insulin, nitroglycerin, liquid antibiotics, and epinephrine auto-injectors degrade quickly. If you use them past their date, you might not get the dose you need. In an emergency, that’s life or death.
On the flip side, most solid pills-like blood pressure meds or antidepressants-stay effective for years if stored properly. A 2015 Mayo Clinic study found 90% of tested drugs were still potent 15 years after expiration. But here’s the catch: your bathroom cabinet isn’t a military storage vault. Heat, humidity, and light wreck stability. The FDA says you should dispose of expired meds. The Institute for Safe Medication Practices says: don’t guess. Check.
A review schedule isn’t about paranoia. It’s about control. It stops you from accidentally taking a degraded drug. It prevents you from buying duplicates because you forgot you had one. And it helps you avoid the $7.2 billion in annual waste from Americans tossing out perfectly good meds out of confusion.
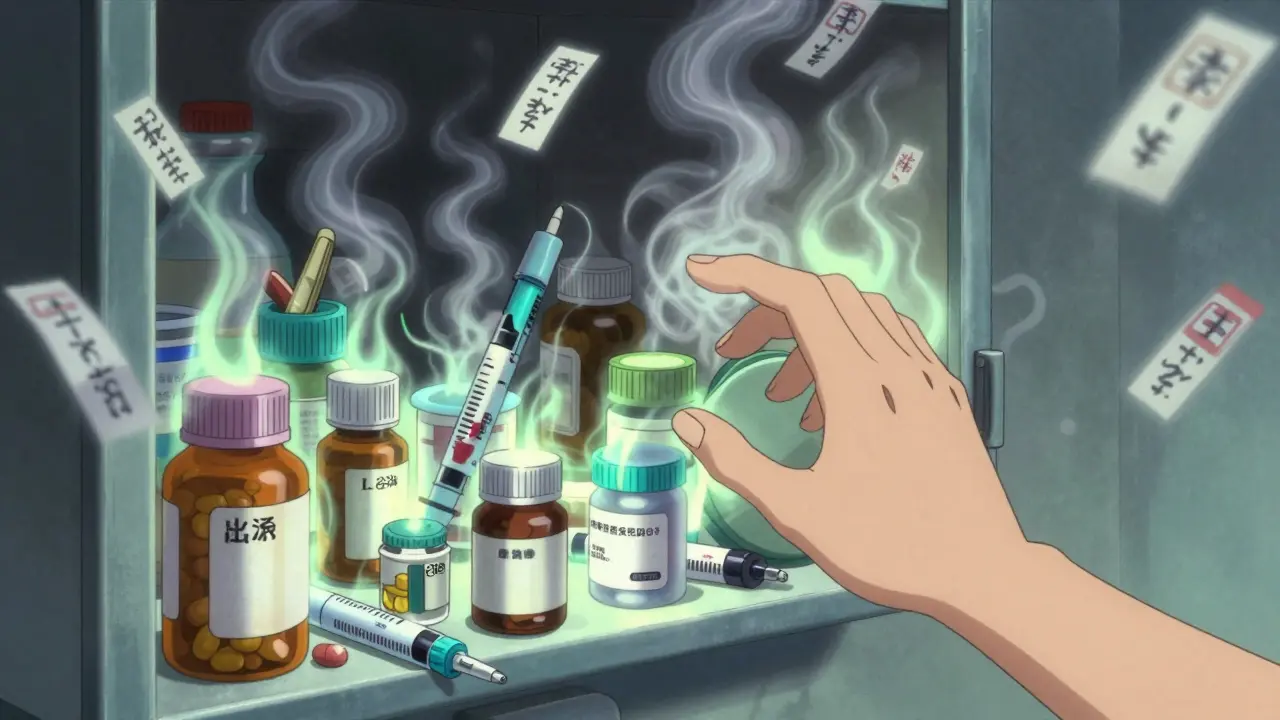
Step 1: Gather Everything
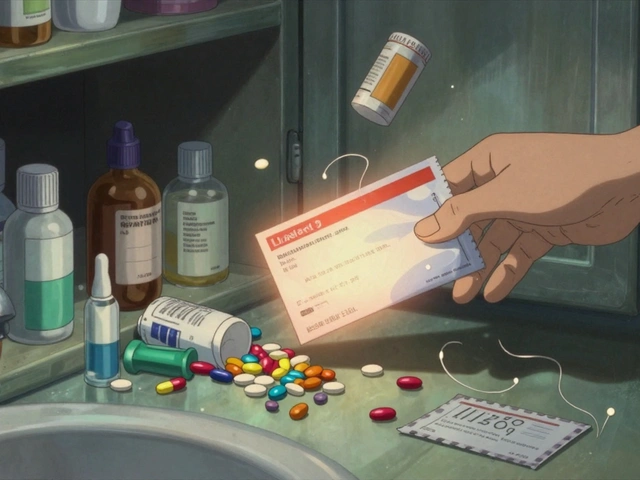
Start by pulling out every medication you have-prescription, over-the-counter, vitamins, supplements. Don’t skip the ones in your car, purse, or gym bag. Check the original packaging. If the bottle’s missing, look for the pharmacy label. If that’s gone too, toss it. No label? No way to know what it is or when it expires.
Write down these details for each item:
- Drug name (e.g., Metformin 500mg)
- Strength and form (tablet, capsule, liquid, inhaler)
- Expiration date (look for “EXP” or “Use by”)
- Prescription number or NDC code (11-digit number on the label)
- Storage condition (room temp, refrigerated, protected from light)
- Quantity remaining
Use a notebook, spreadsheet, or app. Don’t rely on memory. You’ll forget. I’ve seen people keep insulin in the fridge for 18 months past expiration because they thought it was “fine.” It wasn’t.
Step 2: Sort by Risk and Storage
Not all meds are the same. Group them:
- High-risk (check monthly): Insulin, nitroglycerin, epinephrine auto-injectors, liquid antibiotics, eye drops, and any injectables. These can lose potency in weeks after opening or past expiration.
- Medium-risk (check quarterly): Blood pressure pills, diabetes meds, antidepressants, asthma inhalers, birth control. Most are stable, but failure can be serious.
- Low-risk (check twice a year): Pain relievers, antihistamines, antacids, most vitamins. These degrade slowly. Still worth checking, but less urgent.
Also separate by storage:
- Room temperature (68°F-77°F)
- Refrigerated (36°F-46°F)
- Protected from light (in amber bottles or original packaging)
Medications stored in hot, damp places (like a bathroom) expire faster. Move them to a cool, dry drawer. Don’t keep them near the sink or shower.
Step 3: Set Your Review Rhythm
Set calendar reminders. No excuses. Pick a day that sticks-like the first Monday of the month, or your birthday. Make it automatic.
For most people, this works:
- Monthly: Check high-risk meds. Look for discoloration, strange smells, or clumping. If insulin looks cloudy when it should be clear? Toss it. If your epinephrine pen is discolored or has particles? Don’t use it.
- Quarterly: Review medium-risk meds. Cross off anything expired. Note if you’ve used the last dose.
- Twice a year: Scan everything else. Clear out anything you haven’t touched in over a year. If you’re not taking it, you don’t need it.
Use color-coding. Put red stickers on meds expiring in the next 30 days. Yellow for 30-90 days. Green for safe. It’s visual. You’ll notice it.
Step 4: Use Tools That Actually Work
You don’t need fancy tech. But you do need something better than a sticky note.
- Free app options: Medisafe (free version) or MyTherapy. They send alerts, track refills, and log expiration dates. You can even share the list with a family member.
- Simple paper log: Download the National Council on Aging’s free Medication Expiration Log. Print it. Tape it to your fridge. Update it every time you refill.
- Pill organizers: Hero Health or MedMinder. They auto-fill and remind you to take pills. Some even alert you when meds are expiring. Worth the cost if you take 5+ daily meds.
Don’t rely on the pharmacy label alone. Pharmacists print expiration dates based on when the bottle was filled-not when the original bottle expired. That’s why you need your own list.
Step 5: Dispose of Expired Meds Safely
Never flush pills. Never toss them in the trash without mixing them up. The DEA’s National Prescription Drug Take Back Day happens twice a year, but you don’t have to wait.
Here’s how to dispose safely at home:
- Take pills out of their bottles.
- Mix them with coffee grounds, cat litter, or dirt.
- Put them in a sealed bag or container.
- Toss in the trash.
For liquids, don’t pour them down the drain. Mix with absorbent material like sawdust, seal it, and trash it.
Find a drop-off location near you: Visit DEA’s Drug Disposal Locator (or ask your pharmacy). Many CVS, Walgreens, and police stations have secure bins.
What to Do When You’re Not Sure
Ever look at a pill and think, “Is this still good?” Here’s what to do:
- If it’s insulin, nitroglycerin, or epinephrine-throw it out if expired. No exceptions.
- If it’s a solid pill and it looks normal (no cracks, odor, discoloration), and you’ve stored it properly, it’s probably fine. But don’t use it for a life-threatening condition.
- If you’re unsure, call your pharmacist. They’ll tell you for free. Most will even take back unused meds.
Don’t trust Reddit advice. Don’t guess based on how it “looks.” You’re not a chemist. Your job is to stay safe.

Common Mistakes (And How to Avoid Them)
People mess this up in predictable ways:
- “I’ll just use it if I need it.” → You won’t remember the date. Set reminders.
- “It’s still in the original bottle.” → The bottle doesn’t protect it. Heat and light still get in.
- “I can’t afford to throw it away.” → Expired meds don’t work. You’re wasting money on ineffective treatment. A new prescription is cheaper than a hospital visit.
- “My doctor didn’t tell me to check.” → Most doctors don’t. That’s why you need your own system.
One woman in Bristol told me she kept her husband’s heart medication past its date because she didn’t want to “waste it.” He had a heart attack two weeks later. The pill didn’t work. That’s the kind of story you don’t want to be part of.
What Happens If You Don’t Do This?
According to the Agency for Healthcare Research and Quality, 76.4% of home medication errors involve expired drugs. The top offenders? Asthma inhalers, epinephrine pens, and birth control pills. People think they’re fine until they’re not.
Insulin that’s too old? Blood sugar spikes. Epinephrine that’s degraded? Anaphylaxis isn’t stopped. Birth control pills past expiration? Unplanned pregnancy. These aren’t theoretical risks. They’re real, documented events.
And the financial cost? You’re throwing away $7.2 billion worth of usable meds every year because you don’t know what to do. That’s not frugality. That’s ignorance.
Final Tip: Make It a Habit
Do this once. Then make it part of your routine. Link it to something you already do-like paying bills, cleaning out your wallet, or checking your calendar. After two cycles, it’ll feel automatic.
Keep your list updated. Every time you get a new prescription, add it. Every time you finish a bottle, cross it off. Your future self will thank you.
Medication safety isn’t about perfection. It’s about reducing risk. One schedule. One check. One less chance for something to go wrong.





Man, I never thought about how my bathroom is basically a sauna for my pills. I’ve got half my meds in there next to the shower. No wonder my insulin always looks weird. Just moved everything to a drawer under my bed. Felt like a survivalist prepping for the apocalypse, but hey-better safe than sorry. 🤷♂️
Thank you for this detailed guide. I appreciate the emphasis on proper storage conditions-many people overlook humidity and light exposure, which can degrade medications faster than the expiration date suggests. A well-organized system like this is not just prudent, it’s essential for long-term health management.
Expiration dates are a corporate scam designed to keep you buying more pills. The FDA knows most drugs last decades. You’re being manipulated. Just take it. What’s the worst that could happen
I just threw out my entire medicine cabinet last week. All of it. Every bottle. Every capsule. Every sad little vitamin that had been sitting there since 2018. And you know what? I felt FREE. Like I’d shed a skin. Like I’d finally stopped hoarding fear in pill form. 🌿
I’ve been doing this for years. Started after my grandma nearly died from taking old antibiotics. Now I use a spreadsheet with color-coded rows and auto-email reminders every quarter. I even tag the pills with QR codes that link to their original prescription info. It’s overkill? Maybe. But when your life depends on it, ‘maybe’ isn’t good enough. I’ve saved myself over $3,000 in duplicate prescriptions since 2020. And I’ve never once had to rush to the ER because I didn’t know if something still worked.
People think this is paranoia. It’s not. It’s accountability. You wouldn’t drive a car with worn-out brakes and say, ‘Eh, it’s probably fine.’ Why treat your body any differently?
I’ve even started sharing the template with friends. One guy told me he’s now using it for his diabetic father. Another said she finally stopped giving her dog expired heart meds. That one hit me hard. We’re not just managing pills-we’re managing trust. Trust in our own systems. Trust in our own care.
It’s not glamorous. No one posts about it on Instagram. But if you’re reading this and you’ve got a drawer full of mystery capsules? Do yourself a favor. Pull them out. Write them down. Make a plan. Your future self will thank you in ways you can’t imagine right now.
And if you’re worried about cost? Talk to your pharmacist. Most will give you free disposal bags. Some will even refill your meds at a discount if you bring back the old ones. You’re not wasting money-you’re investing in clarity.
This isn’t about being perfect. It’s about being present. And presence? That’s the real medicine.
This is amazing!! 💪 I just started using Medisafe last month and it’s been a game-changer. Got alerts for my blood pressure meds expiring next week-caught it before I ran out! Also started using the NCOA log and taped it to my fridge. My partner even jokes now that our kitchen looks like a pharmacy control center 😆 But honestly? Worth it. I feel so much more in control. If you’re reading this and haven’t started yet-just do it today. One step. One list. One less worry. You got this!! 🙌
Why are you wasting time on this? Just use the pills. The government lies about expiration dates anyway. You’re being manipulated by Big Pharma. Do nothing.
You think you’re safe because you have a schedule? That’s a crutch. Real people don’t need calendars to live. They adapt. They survive. The expiration date is a suggestion written by lawyers. Your body knows what it needs. If you feel fine taking it-then take it. Stop letting bureaucracy dictate your health. You’re not a robot. You’re a human being.
Bro i just use the med app i got from my cousin. It send me alert when the pill be expired. Also i put all my med in one box. No more mess. I don't care about storage temp. I live in Lagos, it hot everywhere. I just take what i need. If i feel sick, i take. If i feel good, i don't. Simple. No spreadsheet. No sticker. No drama.
OMG I JUST REALIZED I’VE BEEN KEEPING MY BIRTH CONTROL IN THE BATHROOM SINCE 2021 😭 I’M SO STUPID. I’M GOING TO THROW EVERYTHING OUT RIGHT NOW. I’M CRYING. I’M SO GUILTY. I’M GOING TO BUY A NEW MEDICINE BOX AND A FAN AND A DEHUMIDIFIER AND A SMART SCALE TO TRACK MY PILL INTAKE. I’M SO SORRY MY BODY. I’M SO SORRY MY FUTURE SELF. I’M SO SORRY EVERYONE WHO HAS EVER HAD TO CLEAN UP AFTER ME.
This is so important!! 💖 I’m from India and here, people often reuse old meds because they can’t afford new ones. But this guide? It’s perfect. I shared it with my mom and my aunties-they’re now using the color-coded system. One of them even took her expired insulin to the pharmacy and got it replaced for free! Small changes, big impact. Let’s keep this conversation going 🙏
There’s something quietly revolutionary about organizing your medicine like this. It’s not about control-it’s about respect. Respect for the science behind the drug. Respect for your own body’s needs. Respect for the fact that you’re worth the effort. Most of us treat our health like an afterthought. This? This turns it into a ritual. A daily act of self-worth. And in a world that’s always screaming at us to do more, to be more-it’s a quiet rebellion to simply care enough to check the date.
wait so you mean the expiration date isnt when it turns into poison?? i thought it was like milk?? lol i just throw it out after the date but now im confused bc my uncle says his blood pressure pills from 2015 still work??
It’s funny how something so simple-checking a date-can feel so overwhelming. We’ve been conditioned to see medicine as this mysterious, external force. But it’s just chemistry. And chemistry doesn’t care about our anxiety. It just reacts. So why do we make it so complicated? Maybe the real problem isn’t the pills. It’s the fear we’ve built around them. This system doesn’t just track expiration dates. It tracks our relationship with our own well-being. And that’s worth more than any pill.