Opioid-Induced Depression Risk Calculator
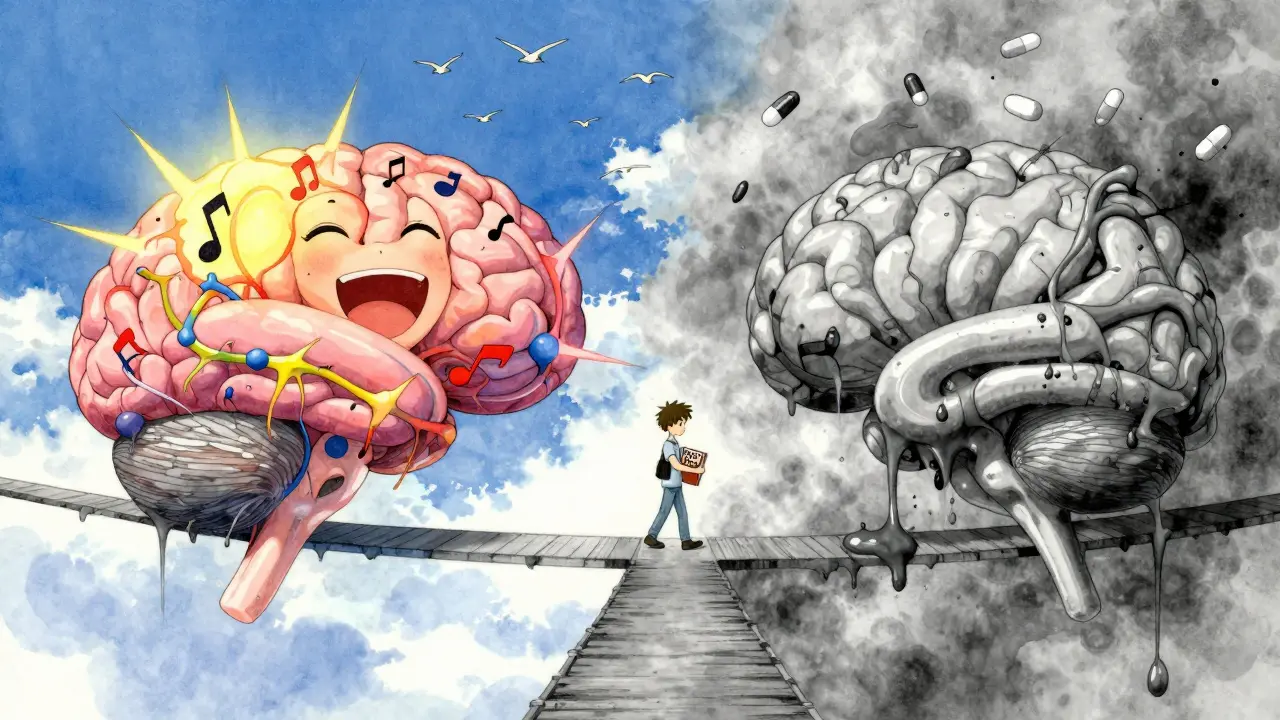
When someone starts taking opioids for chronic pain, they often expect relief from physical discomfort. But many don’t realize that over time, their mood might start to change too - not for the better. It’s not just a coincidence. Opioids and depression are deeply linked, and the connection isn’t always obvious until it’s too late.
Why Opioids Can Make You Feel Worse, Not Better
At first, opioids can feel like they lift your spirits. Pain relief alone can improve mood. But the brain’s reward system doesn’t handle long-term opioid exposure well. Over weeks or months, the body starts to rely on the drug to feel even a little normal. This changes how natural chemicals like dopamine and serotonin work. The result? A slow drop in motivation, pleasure, and emotional resilience - classic signs of depression. Studies show that between 30% and 54% of people with long-term pain also have major depression. And it’s not just that depressed people are more likely to get opioids - the opposite is true too. Research published in JAMA Psychiatry in 2020 used genetic data to show that using prescription opioids doesn’t just correlate with depression - it may actually cause it. People with a higher genetic risk for opioid use were more likely to develop major depressive disorder, even after controlling for other factors.The Dose Makes the Difference
Not all opioid use leads to depression. But the risk climbs sharply with higher doses. A 2016 study of burn patients found that the more morphine equivalent a person received over time, the worse their depression scores became. Those taking more than 50 mg per day had more than three times the risk of developing depression compared to those not using opioids at all. Even small daily use adds up. Another study tracking over 34,000 people found that those using opioids weekly or daily were nearly twice as likely to develop depressive disorders than those using them only once a month or less. This isn’t about addiction - it’s about brain chemistry. Long-term opioid exposure changes how the brain responds to stress, pleasure, and pain signals. The endogenous opioid system, which naturally helps regulate mood, becomes less responsive. That’s when low mood, fatigue, and emotional numbness start to creep in.It’s a Two-Way Street
Depression doesn’t just happen because of opioids - it can also lead to them. People with untreated depression often experience pain more intensely. They may seek out opioids not just for physical relief, but because they’re hoping for emotional relief too. A 2018 study showed that depressed patients are twice as likely to move from short-term to long-term opioid use. And once they’re on long-term opioids, their depression tends to get worse - creating a cycle that’s hard to break. The numbers are sobering. People with major depressive disorder are 2.5 times more likely to develop opioid use disorder. And when both conditions are present, daily life becomes harder. Pain interferes with work, sleep, and relationships 37% more than in those without depression. Mental distress scores are 42% higher. It’s not just about feeling sad - it’s about losing the ability to function.
What to Watch For: Signs of Opioid-Induced Depression
Depression from opioids doesn’t always look like classic sadness. Many people describe it as:- Feeling emotionally flat - nothing excites or moves you anymore
- Loss of interest in hobbies, friends, or even food
- Constant fatigue, even after sleeping
- Difficulty concentrating or making simple decisions
- Increased irritability or anger, especially toward loved ones
- Waking up early and being unable to fall back asleep
How to Monitor Mood Changes Properly
The American Pain Society and the CDC both recommend screening for depression in anyone on long-term opioids. But in practice, only about 40% of doctors do it regularly. That’s a gap that can cost lives. Effective monitoring means using tools like the PHQ-9 (Patient Health Questionnaire-9), a simple 9-item test that takes less than 5 minutes. It asks about sleep, energy, appetite, concentration, and feelings of hopelessness. A score above 10 suggests moderate to severe depression and needs action. But tools alone aren’t enough. Clinicians need to ask open-ended questions:- "How has your mood been since you started this medication?"
- "Have you noticed anything different about what you enjoy or care about?"
- "Do you feel like you’re just going through the motions?"
Can You Treat Depression While Still on Opioids?
Yes - and it often helps both conditions. One of the most promising findings in recent years is that treating depression can reduce opioid use. In the COMBINE trial, patients who received cognitive behavioral therapy (CBT) alongside pain management reduced their opioid doses by 32% over six months. Their pain didn’t get worse - but their mood improved, and they needed less medication. Buprenorphine, a partial opioid agonist used for addiction treatment, has shown surprising antidepressant effects. In one study, patients with opioid use disorder and depression saw their Beck Depression Inventory scores drop from 24.7 (severe) to 13.4 (mild) after three months on buprenorphine. Even low doses - as little as 1-2 mg per day - helped people with treatment-resistant depression in early trials. But here’s the catch: buprenorphine isn’t FDA-approved for depression. That means most doctors can’t prescribe it for this purpose - even if it works. It’s a regulatory roadblock in a field that desperately needs better solutions.What This Means for You
If you’re on opioids for chronic pain, don’t assume your low mood is just part of living with pain. It might be a side effect of the medication. And if you’re depressed and being prescribed opioids, ask: "Could this make my depression worse?" The best approach is proactive. Get screened for depression before starting opioids. Check in with your doctor every month for the first few months. Track your mood with a simple journal - note sleep, energy, and what you feel like doing each day. If you notice your mood slipping, don’t wait. Talk to your provider. Ask about CBT, exercise, or antidepressants that won’t interact badly with your pain meds. You don’t have to choose between pain relief and mental health - you can have both, but you need the right plan.The Bigger Picture
Scientists are still trying to understand why opioids help mood in the short term but hurt it long-term. One theory is that the brain adapts - it stops making its own natural painkillers and mood regulators. Over time, you need more of the drug just to feel normal. That’s when depression sets in. New research is underway. In 2023, the NIH funded a $4.2 million study using brain imaging to track how opioid use changes brain activity in people with depression. Another long-term study tracking 5,000 patients with chronic pain and depression will run through 2026. These projects could lead to better screening tools, safer prescriptions, and even new treatments. For now, the message is clear: opioids aren’t just painkillers. They’re mood-altering drugs. And like any powerful tool, they need careful handling. Ignoring the emotional side effects doesn’t make them go away - it just makes them harder to fix later.Can opioids cause depression even if I take them as prescribed?
Yes. Even when taken exactly as directed, long-term opioid use can alter brain chemistry in ways that lead to depression. Studies show a clear link between higher doses and increased depression risk, regardless of whether the person has a history of mental health issues. It’s not about misuse - it’s about how the brain responds over time.
How long does it take for opioids to affect mood?
Mood changes can start within weeks, but they often become noticeable after 2-3 months of regular use. Some people report emotional numbness or loss of interest as early as 6 weeks. The longer you’re on opioids - especially at higher doses - the greater the risk.
Is it safe to take antidepressants with opioids?
Many antidepressants are safe to use with opioids, but not all. SSRIs like sertraline or escitalopram are commonly used and have few dangerous interactions. However, combining opioids with certain antidepressants like MAOIs can be risky. Always talk to your doctor or pharmacist before starting any new medication. Never adjust doses on your own.
What if I feel better on opioids - does that mean they’re helping my depression?
Feeling better at first doesn’t mean opioids are treating depression. The initial lift often comes from pain relief, not a direct antidepressant effect. Over time, that benefit fades while the risk of depression grows. If your mood improves only while you’re taking the opioid and worsens when you miss a dose, it may be dependence, not treatment.
Should I stop opioids if I’m depressed?
Don’t stop abruptly. Stopping opioids suddenly can cause withdrawal, which worsens depression and anxiety. Instead, talk to your doctor about a plan. You may need to taper slowly while starting a different treatment for pain or depression - like physical therapy, CBT, or non-opioid medications. The goal is to break the cycle safely, not rush out of it.








man i was on oxys for a back injury and didn't realize my mood crashed until i was crying over spilled coffee. felt like i was underwater. docs never asked about my feelings, just kept refilling. big mistake.
The data is unequivocal: opioid-induced neurochemical dysregulation precipitates a cascade of monoaminergic depletion, particularly in the mesolimbic pathway. The 2020 JAMA Psychiatry longitudinal genetic analysis demonstrates a causal relationship, not merely correlation. This is not anecdotal-it is neurobiological fact. Ignoring this mechanism is clinical malpractice.
Look, the West has turned pain into a moral failing. We want magic pills for everything-emotional, physical, existential. Opioids? They’re just the latest symptom of a culture that refuses to sit with discomfort. The brain adapts because we refuse to adapt ourselves. You can’t pharmaceutical your way out of being human.
YOU ARE NOT ALONE. 💔 I felt the same way-empty, tired, like my soul was on mute. But I talked to my pain doc, got on CBT, and slowly, I started laughing again. It took time. It wasn’t easy. But you can get your joy back. I promise. You deserve to feel alive again.
Valid point. But why do doctors ignore PHQ-9? In India, we screen every chronic pain patient. It’s standard. Why is it optional in the US? This is negligence, not healthcare.
People who can’t handle pain shouldn’t be allowed to take opioids. Depression is a character flaw masked as a medical condition. If you’re weak enough to need a pill to feel okay, you’re part of the problem, not the solution.
I get both sides. I was on opioids for 3 years after my accident. Felt great at first. Then I felt nothing. I didn’t want to see friends. I stopped cooking. My wife left. I didn’t realize it was the meds until I tapered. Now I’m on gabapentin and therapy. I’m alive again. It’s not weakness-it’s awareness.
Oh my god, I’ve been there. I was on 80mg of oxycodone daily and felt like I was living in a gray fog. I cried every night. My dog stopped licking my face because I didn’t move. I thought I was broken. Turns out, the drug was. I finally told my doctor and cried for an hour. He cried too. We started buprenorphine. I’m not fixed-but I’m trying. Thank you for writing this. I needed to hear it.
Wow. So now we’re giving out antidepressants like candy and calling it "treatment"? Next you’ll say we should hand out oxy to depressed people because "it helps." At least the old days had discipline. Now? Everyone’s a victim with a prescription.
so like… the brain’s reward system gets hijacked 🤯 and dopamine drops 📉 and suddenly you’re just… numb? like, no joy, no motivation, just… empty? yeah. that’s me. also, buprenorphine is kinda wild bc it’s like a opioid but also not? and it fixes depression?? 🤯🤯🤯 i’m telling my dr tomorrow. #opiodsandmood #brainchemistry
I hate how everyone acts like this is new. I’ve been screaming this for years. They give you a pill for pain and take your soul. I lost my job, my kids, my self. And no one cared until I almost died. Now they want to "monitor"? Too late. The system failed me. And it’s failing you too.