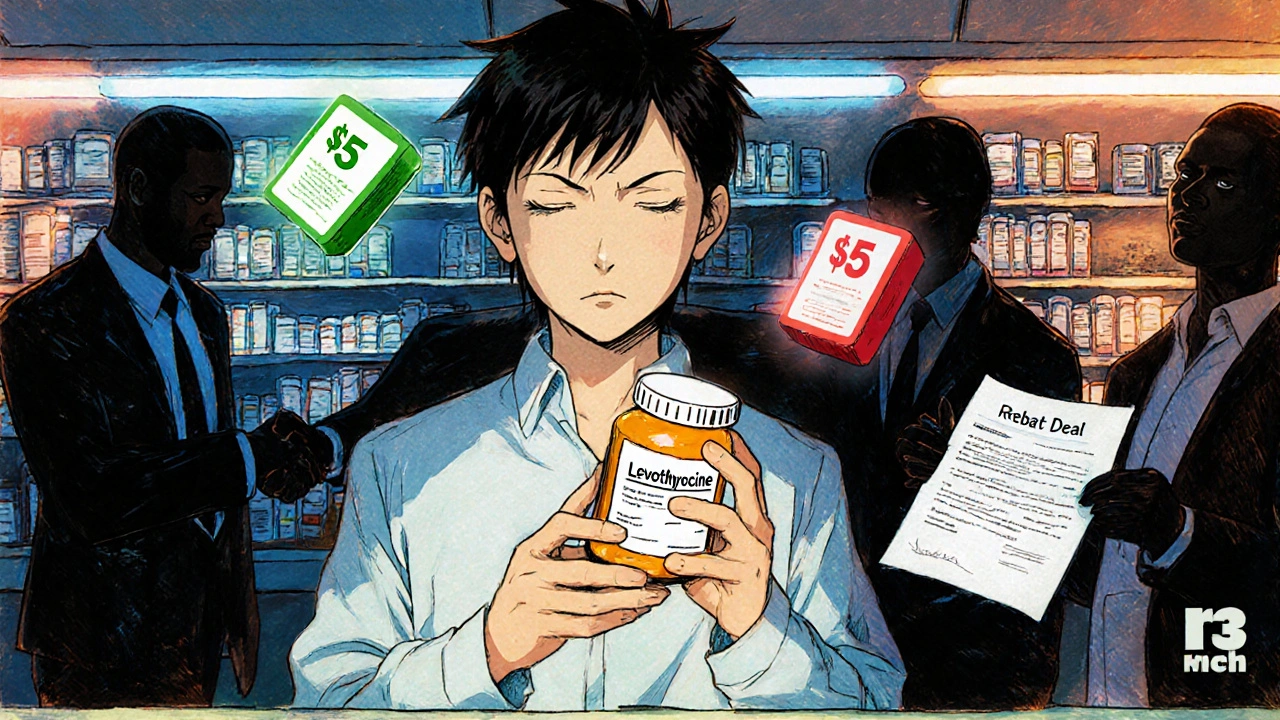
You pick up your prescription for levothyroxine, expecting to pay $5 like last month. But the cashier says $45. You ask why. They shrug. Your doctor says all generics are the same. So why is this one so much more expensive? You’re not imagining it. Your generic drug isn’t broken. The system is.
Not All Generics Are Created Equal-Even When They Are
Generic drugs are supposed to be cheaper versions of brand-name pills. Same active ingredient. Same effectiveness. Same safety. That’s the law. But in your insurance plan, not all generics are treated the same. Some sit in Tier 1 with a $5 copay. Others land in Tier 2 or even Tier 3 with $25, $45, or more. And yes, they’re chemically identical. This isn’t a mistake. It’s by design. Insurance companies and their Pharmacy Benefit Managers (PBMs)-like CVS Caremark, Express Scripts, and OptumRx-use tiered formularies to control spending. They don’t rank drugs based on how well they work. They rank them based on how much money the drugmaker pays them in rebates. If the manufacturer of your generic levothyroxine cuts a deal to give the PBM a big rebate, your drug gets moved to Tier 1. If that deal expires or the manufacturer refuses to play ball, your same pill suddenly jumps to Tier 3. The pill hasn’t changed. Your body hasn’t changed. But your wallet did.How Tiered Copays Actually Work
Most health plans have 4 or 5 tiers. Here’s how they usually break down:- Tier 1: Preferred generics. Usually $0-$15 for a 30-day supply.
- Tier 2: Preferred brand-name drugs. Around $25-$50.
- Tier 3: Non-preferred brand-name drugs. $60-$100.
- Tier 4: Preferred specialty drugs. 20-25% coinsurance.
- Tier 5: Non-preferred specialty drugs. 30-40% coinsurance.
Why Your Insurer Doesn’t Tell You This
Most people assume their insurance plan is designed to help them save money. But the truth? It’s designed to help the insurer save money-and pass some of that savings to you, if it fits their strategy. A 2023 survey found that 41% of insured adults ran into a situation where a generic drug cost more than expected. Of those, 68% said their insurer gave them no clear reason why. Why? Because explaining rebate negotiations isn’t easy. It’s messy. It’s corporate. And it doesn’t make sense to the average person. So instead of transparency, you get silence. Or worse, a pharmacist swaps your prescription without asking. That’s called a therapeutic interchange. The pharmacy substitutes a preferred generic automatically. You don’t know. You don’t get a choice. Then you notice your blood pressure isn’t as controlled, or your thyroid symptoms came back. You blame yourself. But it might be because the new generic, while legal, isn’t the one your body responded to.
What You Can Do About It
You can’t change the system. But you can navigate it. Step 1: Check your formulary. Every plan updates it every October. Log into your insurer’s website. Look up your drug. See what tier it’s on. Write it down. Do this every fall. Step 2: Ask your pharmacist. When you get your prescription, ask: “Is this the preferred generic?” If not, ask: “Is there another version in Tier 1?” Pharmacists know which ones are cheaper. They often can switch it for you. Step 3: Talk to your doctor. If your drug moved to a higher tier, ask your doctor to write a letter requesting a “therapeutic interchange exception.” That’s a formal request to override the tier. In 2024, 63% of these requests were approved. Step 4: Use tools like GoodRx or SmithRx. These apps show you the cash price and the copay across different pharmacies. Sometimes, paying cash is cheaper than using your insurance. Especially for Tier 3 generics. Step 5: Look for manufacturer assistance. Many drugmakers offer coupons or patient assistance programs. Even for generics. You’d be surprised how many cover 20-50% of the cost. Check the drugmaker’s website or call their customer service line.It’s Not Just About Money-It’s About Trust
The biggest problem with tiered copays isn’t the cost. It’s the confusion. Patients feel betrayed. They followed the rules. They took their meds. They trusted their doctor. And now, the same pill costs more because of a contract between two corporations they’ve never heard of. Dr. Aaron Kesselheim from Harvard put it bluntly: “Tiering generics differently undermines the fundamental purpose of generic substitution.” He’s right. Generics were supposed to make medicine affordable. Now, they’re being used as leverage in a financial game. And it’s getting worse. In 2024, Express Scripts moved 87 generic drugs to higher tiers because manufacturer rebates dropped. UnitedHealthcare put some of the most common generics-like atorvastatin and lisinopril-into $0 copay tiers. But only the ones they negotiated with. Others? Upgraded to $10. That’s not saving money. That’s playing favorites.
What’s Next?
The Inflation Reduction Act caps out-of-pocket drug costs at $2,000 a year starting in 2025. That’s huge. But it doesn’t touch tiered formularies. You can still pay $45 for a generic if your plan puts it in Tier 3. The cap just means you won’t pay more than $2,000 total for everything. Some lawmakers want to ban tiering of generics entirely. The bipartisan Prescription Drug Pricing Reduction Act could force insurers to treat all generics the same. But it’s stuck in Congress. For now, the system stays. And you’re left figuring out how to play it.What to Remember
- A generic drug’s price has nothing to do with how well it works. It’s about rebates. - If your generic suddenly costs more, it’s not you. It’s the contract. - Pharmacists can help you find cheaper versions-ask them. - Your doctor can request an exception. It works more often than you think. - Use GoodRx. Sometimes cash beats insurance. - Check your formulary every October. Changes happen. You’re not alone. Millions of people are confused by this same system. But you’re not powerless. You just need to know how to look-and ask.Why is my generic drug more expensive than the brand-name version?
It’s rare, but it happens. Sometimes, the brand-name drug is on a preferred tier because the manufacturer pays a big rebate to the pharmacy benefit manager (PBM). Meanwhile, your generic might be on a higher tier because the maker didn’t negotiate a good deal. The brand may be cheaper than your generic simply because of a corporate contract-not because it’s better.
Can I switch to a different generic to save money?
Yes. Ask your pharmacist if there’s another generic version of your drug that’s in Tier 1. Many drugs have multiple generic manufacturers. One might be preferred, another isn’t. The pills are identical, but the copay isn’t. Your pharmacist can often swap it without needing a new prescription.
What’s a therapeutic interchange exception?
It’s a formal request from your doctor asking your insurance to cover a drug even if it’s not on the preferred tier. You need a letter explaining why the preferred option isn’t right for you-maybe it caused side effects, or you’ve been stable on this one. About 63% of these requests are approved in 2024.
Do all insurance plans use tiered copays?
Almost all do. 98% of employer plans and 99% of Medicare Part D plans use tiered formularies. Flat copays (same price for everything) are nearly gone. Tiering is the standard because it helps insurers manage costs-and PBMs make billions from the rebates tied to these tiers.
Are specialty generics really different?
Yes, but not because they’re stronger. Specialty generics are high-cost drugs used for complex conditions like rheumatoid arthritis or multiple sclerosis. Even if they’re generics, they’re often placed in Tier 4 or 5 because they cost over $600 a month, require special handling, or need prior authorization. That’s why your $500-a-month generic for adalimumab has a 30% coinsurance. It’s not clinical-it’s financial.
Why don’t insurers just make all generics Tier 1?
Because they make money by steering patients toward drugs that pay them the biggest rebates. If every generic cost $5, drugmakers wouldn’t need to offer discounts. Tiering creates pressure to negotiate. The more tiers, the more control insurers have over which drugs get used. It’s a business model, not a health policy.








This system is rigged. I pay for insurance so I don't have to play financial roulette just to get my thyroid meds.
The conflation of chemical equivalence with economic equivalence is a systemic failure of epistemology in pharmaceutical policy. The state sanctions a fiction: that cost reflects value. It does not. It reflects negotiation power.
STOP accepting this! You have POWER. Check your formulary. Ask your pharmacist. Demand an exception. Your health isn't a spreadsheet. Fight back. You're not alone. This is fixable.
generic drugs r not even the same i read on a forum that some have diff fillers that make u feel weird like brain fog or dizzy. no one talks about this
My pharmacist just swapped my pill without telling me. I felt like a lab rat. This is wild.
The PBM rebate architecture creates perverse incentives that undermine therapeutic continuity. We need structural reform, not just individual workarounds.
Just checked my formulary-my levothyroxine jumped to Tier 3 last month. I called my doc and got an exception approved in 2 days. You can do this. Don't give up.
Big Pharma + PBMs = one giant scam. They're all in cahoots. You think this is about health? Nah. It's about who owns your body. 🕵️♂️
GoodRx saved me $38 last month on my lisinopril. Cash price was $12. Insurance copay was $50. I didn't even know this was a thing until my buddy told me. Seriously, check it out.
As someone from a country where meds are subsidized, this feels insane. But I'm glad people are talking about it. Change starts with awareness.
Wait-so the FDA says generics are bioequivalent, but the PBM says only one version is "preferred"? That’s not a health policy-it’s a market manipulation scheme. And we’re supposed to just... accept this?!
I had the same thing happen with my antidepressant. Switched to a different generic and felt like crap for weeks. Turns out my body just needed the old one. Never assume they're all the same.
Physicians are often unaware of tier changes until patients present with billing issues. Proactive formulary review should be standard practice during annual visits.