Every year, more people die from lung cancer than from breast, colon, and prostate cancer combined. And for smokers, the risk doesn’t just go away after quitting-it lingers for years. But here’s the good news: if you’re in a high-risk group, a simple, quick scan can catch lung cancer early, when it’s most treatable. That scan is called low-dose CT, or LDCT. It’s not a cure. It’s not a magic bullet. But for people who’ve smoked for years, it’s one of the most effective tools we have to stay alive.
Who Should Be Screened?
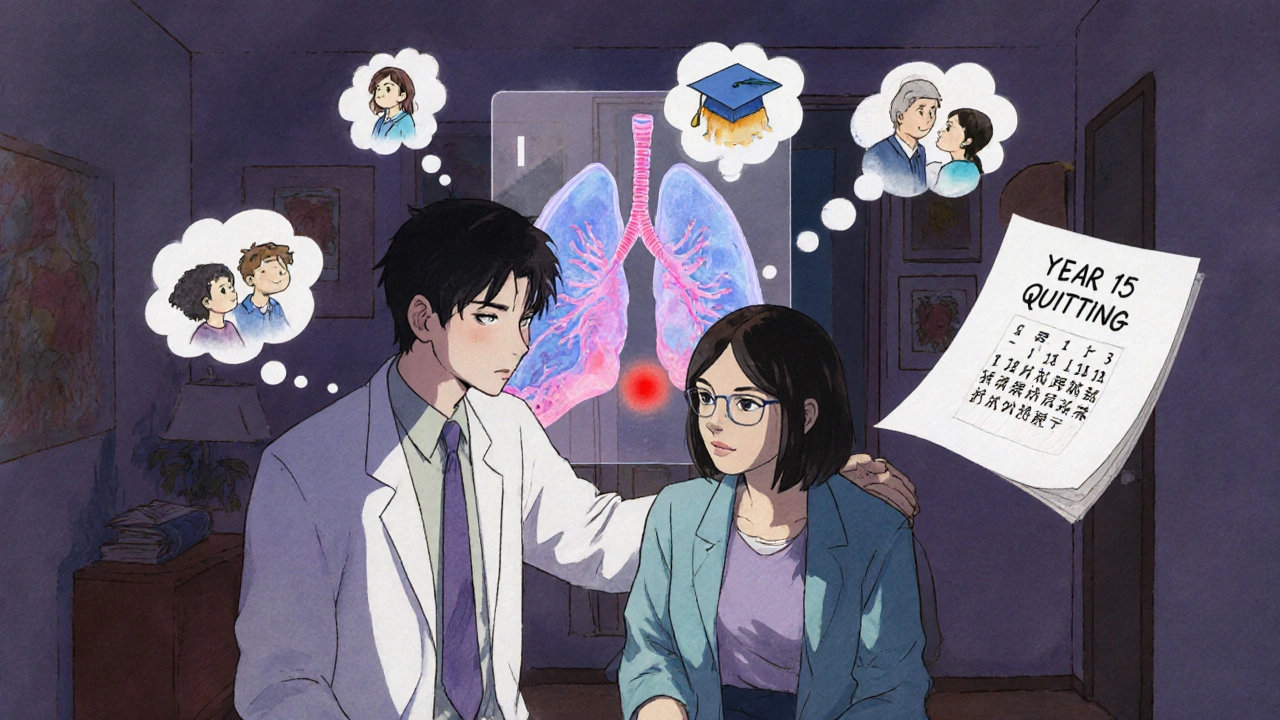
The rules changed in 2021, and they’re now much more inclusive. If you’re between 50 and 80 years old, and you’ve smoked at least 20 pack-years, you qualify. A pack-year means smoking one pack a day for a year. So if you smoked a pack a day for 20 years, or two packs a day for 10 years, you hit the threshold. Even if you quit smoking, you’re still eligible if it’s been less than 15 years since you stopped.Before 2021, the cutoff was 55 to 80 with a 30-pack-year history. That left out millions of people who were still at risk. The update was based on solid data from the National Lung Screening Trial, which showed a 20% drop in lung cancer deaths among those screened with LDCT instead of chest X-rays. That’s not a small win. It’s life-saving.
But here’s the catch: screening stops when you’ve been smoke-free for 15 years, or if you have other health problems that make surgery unlikely. That’s not about giving up. It’s about focusing resources where they’ll do the most good.
How Does Low-Dose CT Work?
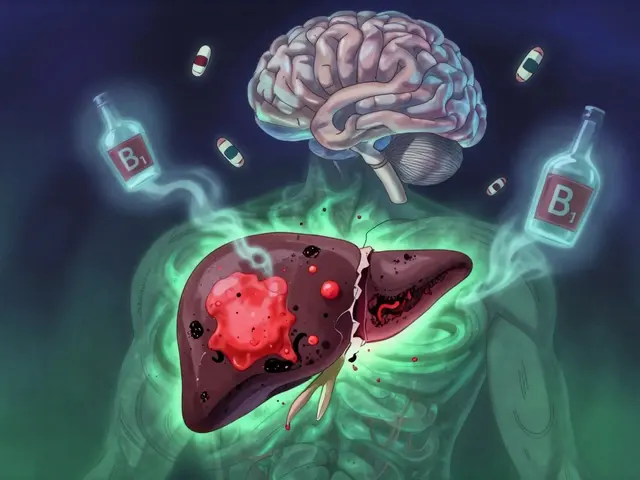
It’s faster than you think. You lie on a table, take a breath, hold it for a few seconds, and that’s it. The whole thing takes under 10 minutes. No needles, no fasting, no prep. The machine uses about 1.5 millisieverts of radiation-roughly a third of what a regular CT scan gives you, and less than what you’d get from a year of natural background radiation in some places.The scan doesn’t just take a picture. It builds a 3D map of your lungs, showing tiny nodules or changes you’d never feel. That’s the power of LDCT. It finds tumors smaller than a pea, often before they spread.
But finding something doesn’t always mean it’s cancer. About 1 in 7 people who get screened will have a result that looks suspicious. That’s called a false positive. Most of the time, it’s just scar tissue, inflammation, or a harmless nodule. Still, it leads to more tests-another scan, a biopsy, sometimes even surgery. That’s stressful. And that’s why the conversation before screening matters just as much as the scan itself.
The Real Risks and Rewards
Let’s talk numbers. For every 1,000 people screened annually for 5 years, about 3 to 4 lung cancer deaths are prevented. That’s not a huge number on paper. But for the person who gets that early diagnosis? It means they might live to see their grandkids graduate. It means they don’t have to go through chemo or radiation after the cancer has spread.But there’s a flip side. False positives cause anxiety. One study found that 37% of people with false results felt moderate to severe anxiety for over six months. Some people end up with unnecessary procedures that carry their own risks. And while the radiation from LDCT is low, getting it every year for 30 years adds up. That’s why screening isn’t for everyone.
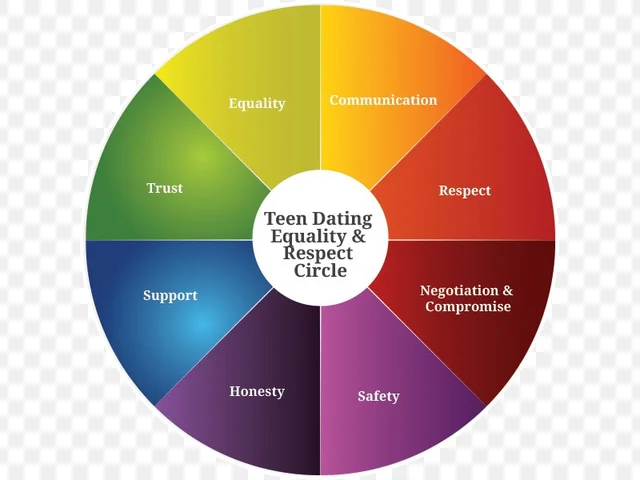
That’s why guidelines stress a shared decision-making visit. Your doctor shouldn’t just hand you a referral. They need to sit down with you-20 to 30 minutes-and explain: Here’s what we might find. Here’s what happens if we find something. Here’s what happens if we don’t. You need to know the trade-offs before you say yes.

Why So Few People Get Screened
Here’s the hard truth: even though millions qualify, fewer than 1 in 10 actually get screened. Why?First, many don’t know they’re eligible. A Medicare survey found 68% of eligible people didn’t realize they qualified. Second, doctors don’t always bring it up. In 42% of cases, the patient never heard a word about screening from their provider. Third, access is a mess. In rural areas, you might have to drive 100 miles to the nearest accredited center. And even if you get the scan, follow-up care isn’t always easy to find.
There’s also a stigma. Some smokers feel guilty. They think, “I brought this on myself,” so they avoid screening. Others don’t think they’re sick enough to need it. But lung cancer doesn’t wait for symptoms. By the time you cough up blood or can’t catch your breath, it’s often too late.
What Happens After the Scan?
Results are scored using something called Lung-RADS. It’s a standardized system that tells your doctor what to do next.- Lung-RADS 1: Nothing found. You come back next year.
- Lung-RADS 2: Benign findings. Still no action needed.
- Lung-RADS 3: Probably benign, but a follow-up scan in 6 months is recommended.
- Lung-RADS 4: Suspicious. You’ll need a diagnostic CT, PET scan, or biopsy.
Most people fall into categories 1 or 2. Only about 1 in 100 will need a biopsy. But when you’re the one waiting for results, it feels like the whole world is on pause.
Some clinics have nurse navigators-specialists who guide you through the process. They schedule follow-ups, answer questions, and help you understand your options. That kind of support can make all the difference.
Who’s Not Getting Screened-and Why It Matters
Black Americans are 20% less likely to get screened than white Americans, even though they have higher lung cancer rates. That gap isn’t random. It’s tied to access, trust, income, and how often doctors talk to their patients about prevention. If you’re poor, live in a food desert, or don’t have a regular doctor, screening is the last thing on your mind.That’s why expanding eligibility was so important. More people qualify now, but unless we fix the system, those same people won’t get the care they need. Screening isn’t just about technology. It’s about equity.
The Future: AI and Better Risk Tools
The field is moving fast. In 2023, the FDA cleared the first AI tool for LDCT analysis-LungAssist by VIDA Diagnostics. It helps radiologists spot nodules faster and reduces false positives by over 15%. That means fewer unnecessary biopsies and less anxiety for patients.There’s also a new risk model called PLCOm2012. It doesn’t just look at pack-years. It adds in family history, education level, and even chronic cough. That could help identify who’s at highest risk, so we can target screening even more precisely.
Right now, screening rates are still stuck at around 8%. The goal is 80%. We’re nowhere close. But every person who gets screened is one more life saved.
What You Can Do
If you’re 50 to 80 and you’ve smoked 20 pack-years or more:- Ask your doctor about LDCT screening. Don’t wait for them to bring it up.
- Ask for a shared decision-making visit. Make sure you understand the risks and benefits.
- If you’re on Medicare, you’re covered-no copay, no deductible.
- Find an ACR-accredited center. You can search online or ask your provider.
- If you’re still smoking, talk to your doctor about quitting. Screening helps, but quitting saves more lives.
Screening isn’t about fear. It’s about control. You can’t undo your past. But you can protect your future.
Who qualifies for lung cancer screening with low-dose CT?
You qualify if you’re between 50 and 80 years old, have a smoking history of at least 20 pack-years (like one pack a day for 20 years), and currently smoke or quit within the past 15 years. Screening stops after 15 years of not smoking or if you have serious health issues that make treatment unlikely.
Is low-dose CT the same as a regular CT scan?
No. A low-dose CT (LDCT) uses about 1.5 millisieverts of radiation-much less than a standard CT, which can use 7 to 8 millisieverts. It’s designed to find small lung nodules without exposing you to high radiation. It’s faster, safer, and optimized for screening, not detailed diagnosis.
What if my scan shows a nodule?
Most nodules are not cancer. About 13.9% of screenings show something suspicious, but only about 1 in 100 lead to a biopsy. If a nodule is found, your doctor will use the Lung-RADS system to decide if you need a follow-up scan in 3, 6, or 12 months-or if you need further testing like a biopsy. Anxiety is common, but most findings turn out to be harmless.
Does Medicare cover low-dose CT screening?
Yes. Medicare covers annual LDCT screening for people aged 50 to 77 who meet the smoking history criteria. You need a referral from your provider after a shared decision-making visit. There’s no copay or deductible if the provider accepts Medicare assignment.
Why don’t more people get screened if it saves lives?
Many people don’t know they qualify. Others don’t have a doctor who brings it up. Access is limited in rural areas, and transportation is a barrier. There’s also fear of false positives and stigma around smoking. Only about 8% of eligible people get screened, despite the proven benefit.
Can AI help improve lung cancer screening?
Yes. In 2023, the FDA approved the first AI tool for LDCT analysis-LungAssist by VIDA Diagnostics. It helps radiologists detect nodules more accurately and reduces false positives by over 15%. This means fewer unnecessary biopsies and less anxiety for patients. AI isn’t replacing doctors-it’s helping them work faster and more precisely.




So we’re just gonna scan everyone who ever smoked and call it a day? What about the people who never smoked but got lung cancer from secondhand smoke, radon, or just bad luck? This feels like a band-aid on a bullet wound. We’re treating the symptom, not the cause. And don’t even get me started on how this just reinforces the idea that smokers are disposable-‘here’s your scan, now go quit, but we’re not fixing air quality or tobacco taxes.’
The LDCT protocol, while statistically significant in cohort studies, suffers from high false-positive rates (14.3% per the NLST meta-analysis), leading to unnecessary PET-CTs and biopsy-related complications, including pneumothorax and mediastinitis. Moreover, the cost-benefit ratio deteriorates significantly in populations with comorbidities like COPD or cardiovascular disease, where life expectancy is truncated. Screening is not a panacea-it’s a risk stratification tool with nontrivial downstream burdens.
Let’s be real-this whole screening push is just another government handout for people who made terrible life choices. If you smoked for 20 years, you knew the risks. Now you want the system to save you? Meanwhile, my dad died of lung cancer at 52 and he never touched a cigarette. He worked in a factory. No scans for him. No pity. Just reality. We’re rewarding bad behavior and punishing the responsible.
My uncle got screened last year and they found a nodule 😳 Turned out it was just a scar from an old pneumonia. But the anxiety?? I swear I aged 5 years waiting for results. Still, I’m telling everyone I know to get it done. Better safe than sorry 🙏 #LungCancerAwareness
why do they keep saying 20 pack years like its some magic number? i smoked 15 years but 2 packs a day so thats 30 and i quit 12 years ago… so im still good right? or do they just not care about people like me? also why is it so hard to find a place that does this??
I got screened last year after my doctor finally brought it up. I smoked for 22 years, quit 8 years ago. They found nothing. I feel like I won the lottery. But I didn’t just get lucky-I asked. I made sure to get that shared decision visit. If you’re eligible, don’t wait. Talk to your doctor. It’s free with Medicare. Seriously, do it.
Let’s be honest: this is just another bureaucratic checkbox. The ‘shared decision-making visit’? That’s a 20-minute lecture delivered by a resident who’s never smoked and doesn’t care. Meanwhile, the real problem is the lack of primary care access in rural America. You can’t screen people who can’t get to a clinic in the first place. And AI? Cute. But it doesn’t fix Medicaid underfunding or the fact that 40% of eligible patients don’t have a PCP.
What’s interesting is how this screening program forces us to confront a deeper question: What do we owe people who made harmful choices? Is healthcare a right, or a reward for virtue? The answer isn’t in the scan-it’s in how we treat people after they walk out of the clinic. If we just hand them a referral and call it justice, we’re missing the point. Screening is a tool, but dignity is the foundation.
Okay, but the AI thing? LungAssist? I’ve seen the data-it’s not just reducing false positives, it’s cutting down radiologist burnout. We’re talking about a 22% reduction in time per scan. That means more scans done, faster turnaround, less anxiety. This isn’t sci-fi-it’s happening right now. And yeah, it’s still imperfect, but it’s a leap forward. We need more tools like this, not less.
I’m 56, smoked for 18 years, quit 10 years ago. I didn’t know I qualified until I read this. I’m scheduling my scan this week. No drama. Just… thank you for writing this. I needed to hear it.
Hey, if you’re reading this and you’re even thinking about getting screened-just do it. I know it’s scary. I was terrified too. But I got mine last year and it was over before I could panic. No needles, no fasting, no big deal. And if you’re still smoking? Talk to your doctor about quitting. Screening helps, but quitting? That’s the real win. You’ve got this 💪
Oh wow. So now we’re scanning people who smoked 20 years ago? What’s next? Scanning people who drank soda? Or ate fast food? Let’s just turn every hospital into a cancer-detection factory and call it ‘preventative care.’ Brilliant.
Let’s not forget: the NLST trial was funded by the NIH, and the ACR guidelines were written by radiologists who stand to profit from increased scan volume. This isn’t science-it’s a revenue stream disguised as public health. And don’t get me started on the ‘no copay’ nonsense-Medicare’s paying for it, which means YOU are.