Statins Side Effect Risk Calculator
Personalized Risk Assessment
This tool estimates your risk of common statin side effects based on gender-specific factors. Results are for informational purposes only and should not replace professional medical advice.
Personalized Risk Assessment
Muscle Pain Risk
Diabetes Risk
Recommendations
Women take statins for the same reason men do: to lower cholesterol and reduce the risk of heart attacks and strokes. But the way their bodies react to these drugs is different-and often more challenging. While statins save lives, many women stop taking them because of side effects that are more common, more severe, and less understood than in men. This isn’t about being overly sensitive. It’s biology. And it’s time we treated it that way.
Why Women Get More Muscle Pain
Muscle pain is the #1 reason women quit statins. Studies show 31% of women report new or worsening muscle aches, compared to just 26% of men. That might not sound like a big difference, but when you look at what happens next, it’s alarming. Women are nearly 30% more likely to stop taking statins because of it. And it’s not just a minor nuisance-it can be debilitating enough to keep someone from walking, climbing stairs, or even getting out of bed. The reason? It’s not just about how much you weigh or how active you are. Women naturally have lower kidney function-about 15-20% less than men after adjusting for body size. That means statins stay in the body longer. Women also tend to have higher body fat percentages (25-30% on average vs. 15-20% in men), which changes how the drug is absorbed and distributed. The result? Higher exposure to the medication, and a higher chance of muscle damage. This gets worse with age. Women over 65 are 1.5 to 2 times more likely than men their age to develop statin-induced myopathy. Why? Because older women are more likely to be on multiple medications-like blood pressure pills or blood thinners-that interact with statins. One common combo: simvastatin and calcium channel blockers. Together, they can increase toxicity risk by 300%.Higher Risk of Developing Diabetes
Statins can raise blood sugar levels. The FDA added this warning in 2012, and since then, studies have confirmed it. For every 100 people taking statins for four years, about 9-12 will develop type 2 diabetes. But here’s the catch: women seem to be at slightly higher risk than men. Some analyses suggest a 12% increase in diabetes risk for women versus 8% for men. And it doesn’t matter which statin you take. Whether it’s atorvastatin, rosuvastatin, or simvastatin-the risk is there. A 2013 study in the Journal of the American College of Cardiology found that post-menopausal women taking any statin for three years or more had a measurable rise in blood sugar, regardless of dose. That’s why doctors should check fasting glucose every 3 to 6 months in women on long-term statin therapy. But here’s the critical part: the diabetes risk is still far smaller than the heart attack risk statins prevent. For a woman with high cholesterol and a family history of heart disease, skipping statins because of diabetes fears is like avoiding a seatbelt because you’re worried about a bruise.Doctors Don’t Talk to Women About This
Here’s a harsh truth: many women aren’t warned about these risks before they start statins. A 2019 study found that 42% of women said their doctor never explained how high cholesterol leads to heart disease. Compare that to 31% of men. That gap isn’t random. It’s bias. When women report muscle pain, fatigue, or brain fog, they’re more likely to be told it’s “just stress,” “aging,” or “not related to the pill.” Meanwhile, men with the same symptoms are more often taken seriously. This isn’t just frustrating-it’s dangerous. Women who feel unheard are less likely to stick with treatment. One survey showed women are 2.3 times more likely than men to try three or more different statins before finding one they can tolerate. And when statins don’t work? Women are 37% less likely to be offered alternatives like ezetimibe or PCSK9 inhibitors. These are effective, non-statin options that don’t cause muscle pain. But many providers never mention them. Why? Because they assume statins are the only tool-and that women will just “get used to it.”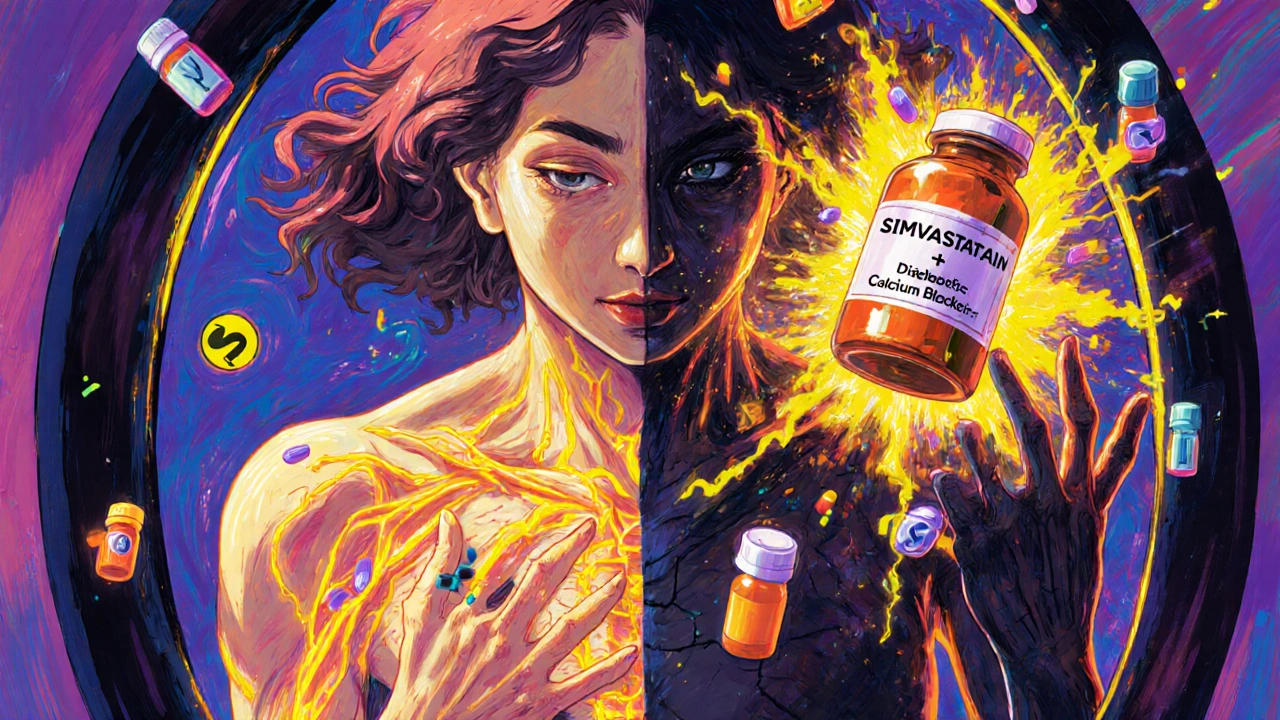
Women Are Less Likely to Even Get Prescribed Statins
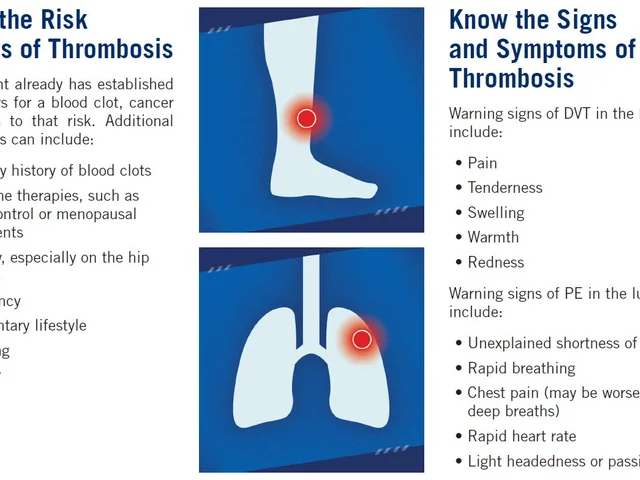
Even when women qualify for statins based on guidelines, they’re less likely to get them. In one analysis of over 5,600 patients, only 67% of women who met criteria were prescribed statins-compared to 78% of men. This gap stays even after a heart attack. It’s not because women are less at risk. It’s because the system still treats heart disease as a “man’s problem.” Historically, clinical trials for statins included far fewer women. A 2012 review of 18 major trials with over 140,000 people found that while statins worked equally well in both sexes, most of the data came from men. So guidelines were built on male biology. That’s like designing car seats based only on male body shapes and wondering why women get hurt more in crashes.What Happens During Menopause and After 75?
Menopause changes everything. As estrogen drops, cholesterol rises-and so does heart disease risk. But at the same time, muscle pain from statins becomes more common. The Women’s Health Initiative found that 41% of post-menopausal women reported muscle symptoms, compared to 33% of younger women. And for women over 75? The risk spikes again. A 2021 study of Medicare patients found that women in this age group were more than twice as likely as men to be hospitalized for serious statin side effects. Why? Polypharmacy. Elderly women often take 5-7 medications daily. Statins interact with common drugs like warfarin, amiodarone, and even some antibiotics. These interactions can turn a safe dose into a dangerous one.What Can Women Do?
You don’t have to suffer through side effects. There are better ways. Start low, go slow. Instead of jumping to 20mg of atorvastatin, start with 10mg. A 2020 Dutch trial showed this approach improved adherence by 32% in women. Give your body time to adjust. Ask about genetic testing. A gene called SLCO1B1 affects how your body processes statins. About 23% of women carry a variant that increases muscle pain risk. A simple blood test before starting can help your doctor pick a safer statin-like pravastatin or fluvastatin-instead of simvastatin or rosuvastatin. Request alternatives. If muscle pain persists, ask about ezetimibe or PCSK9 inhibitors. These lower LDL without touching muscles. They’re not cheap, but they work-and they’re worth it if statins aren’t. Track your numbers. Get fasting glucose checked every 3-6 months. Keep a symptom journal: when did the pain start? Did it get worse after changing doses? Did it go away after skipping a dose? Bring this to your doctor. Insist on communication. If your doctor doesn’t explain why you need statins, ask again. Say: “I want to understand my real risk of heart disease and how this pill helps.” If they brush you off, find someone who listens.
It’s Not Just About the Pill
Statins aren’t magic. They work best with lifestyle changes. But women are often expected to do all the work-eat better, exercise more, manage stress-while being told the pill is the solution. That’s unfair. The real fix? A system that acknowledges women’s biology, listens to their symptoms, and offers real choices. It’s not about being “difficult.” It’s about being human.Frequently Asked Questions
Do statins cause weight gain in women?
Statins themselves don’t directly cause weight gain. But some women report increased appetite or fatigue that makes exercise harder, which can lead to weight gain over time. Muscle pain from statins may also reduce physical activity, indirectly affecting weight. If you notice unexplained weight gain, talk to your doctor-it could signal another issue like thyroid problems or insulin resistance.
Can I take statins if I’m planning to get pregnant?
No. All statins are classified as Pregnancy Category X, meaning they can cause birth defects. If you’re planning pregnancy or could become pregnant, your doctor should discuss reliable contraception before starting statins. If you become pregnant while taking one, stop immediately and contact your provider. Statins are not safe during pregnancy, breastfeeding, or if you’re trying to conceive.
Are natural supplements like red yeast rice safer than statins for women?
Red yeast rice contains a compound similar to lovastatin, one of the first statins. That means it carries the same risks-muscle pain, liver issues, and drug interactions-but without the safety testing, quality control, or dosage standardization of prescription statins. It’s not safer. It’s unregulated. Many products on the market have inconsistent amounts of active ingredients or even contaminants. Stick with FDA-approved medications and talk to your doctor before trying supplements.
Why do some women feel mentally foggy on statins?
Some women report memory issues or brain fog, though large studies haven’t proven a direct link. Statins lower cholesterol, which the brain needs to make connections. A small number of people may be sensitive to this change. If you notice mental changes, don’t assume it’s normal. Talk to your doctor. Sometimes switching to a different statin (like pravastatin, which doesn’t cross the blood-brain barrier as easily) helps. Never stop cold turkey without medical advice.
Is it true that women are more likely to stop statins than men?
Yes. Studies show women are 28.7% more likely than men to stop or switch statins due to side effects. Muscle pain is the top reason, but poor communication, lack of alternatives, and being dismissed by providers also play big roles. This isn’t about compliance-it’s about care. When women feel heard and supported, adherence improves dramatically.





Hey, just wanted to say this article hit home. I started statins last year and thought my muscle pain was just from aging-turns out it was the drug. Started at 10mg of pravastatin like they suggested and now I’m hiking again. Don’t let anyone tell you to just tough it out. Your body talks-you just gotta listen.
Also, glucose checks? Do them. Mine spiked after 6 months. Caught it early. No diabetes. Just a wake-up call.
OMG YES I’M SO GLAD SOMEONE FINALLY SAID THIS!!! I was told my fatigue was ‘just stress’ for 8 months until I demanded a statin review. Switched to ezetimibe and I feel like a new person. Why do docs act like women are just being dramatic???
Anne, you’re a legend. 🙌 I literally just texted my doctor this morning after reading this-‘Hey, can we talk about non-statin options? I’m not a martyr.’ He actually listened. Small wins.
Also-red yeast rice? No thanks. I don’t need a mystery supplement giving me liver issues on top of statin pain. FDA-approved = less guesswork. 🙏
Interesting how the article frames this as a gendered issue. But isn’t this just another case of conflating correlation with causation? Women live longer. More meds. More polypharmacy. More side effects. It’s not biology-it’s dosage accumulation.
Also, ‘heart disease is a man’s problem’? That’s a tired narrative. The data doesn’t support systemic sexism-it supports underdiagnosis in younger women. Big difference.
Oh here we go again. ‘Women’s biology’ this, ‘systemic bias’ that. Can we please stop pretending women are fragile lab rats? I’ve been on statins for 12 years. No muscle pain. No diabetes. I don’t need a 3000-word essay telling me my body is broken.
Also, ‘ask for genetic testing’? Great. Now I’m supposed to pay $500 to avoid a drug that might not even hurt me? What a scam.
From a clinical pharmacology standpoint, the SLCO1B1 polymorphism is indeed a major confounder in statin-induced myopathy, particularly in East Asian and South Asian populations where the variant allele frequency exceeds 20%. The pharmacokinetic profile of simvastatin-being highly lipophilic and CYP3A4-metabolized-exacerbates this in women due to lower hepatic clearance and higher adipose tissue sequestration.
Moreover, the estrogen-mediated downregulation of OATP1B1 transporters in postmenopausal women further reduces hepatic uptake, leading to elevated plasma concentrations. This is not merely ‘bias’-it’s pharmacogenomic reality. The solution? Pre-prescription genotyping, lower starting doses, and non-statin LDL-lowering agents like bempedoic acid or inclisiran where indicated.
I stopped statins after 3 weeks. My legs felt like concrete. My brain? Gone. My doctor said ‘it’s all in your head.’
Turns out it wasn’t.
I’m alive. But I’ll never trust a doctor again.
Ugh. I’m so tired of women being treated like broken machines that need ‘fixing’-but only if they’re quiet about it. I had a doctor tell me I was ‘too emotional’ to be on statins. TOO EMOTIONAL?? I was in PAIN. I couldn’t carry my groceries. I was 58, not 98.
So I switched to ezetimibe. No muscle pain. No brain fog. No ‘it’s just stress.’
And guess what? My LDL is lower than when I was on rosuvastatin.
Women aren’t ‘difficult.’ We’re just done being ignored.
Let’s cut the crap. This isn’t about biology. It’s about feminism turning every medical issue into a gender war. Statins work. Women take them. Some get side effects. Men get them too. Stop making it political. Just test, adjust, and move on. No drama. No hashtags. Just science.
There's a quiet truth here that doesn't make headlines: medicine was built for a male body and we're still trying to retrofit it for everyone else. The fact that we're only now noticing women's different responses to statins isn't proof of negligence-it's proof of how long we've been looking through the wrong lens.
It's not about blame. It's about awareness. And awareness, slowly, is changing practice. I've seen it in my clinic. More genetic screening. More alternatives offered. More listening.
Change doesn't happen with rage. It happens with data. And this article? It's data with a heartbeat.