By 2027, more than half of all generic medications in the U.S. will be delivered through digital pharmacy platforms. That’s not a guess-it’s what Deloitte predicts based on current adoption trends, technological breakthroughs, and patient demand. The shift isn’t just about convenience. It’s about fixing broken systems: long waits, hidden costs, and pharmacy deserts where millions can’t get basic meds. Digital pharmacy isn’t replacing your local pharmacist-it’s giving them superpowers.
How Generic Medications Became the Core of Digital Pharmacy
Generic drugs make up 90% of all prescriptions filled in the U.S., according to FDA data from 2022. They’re cheaper, just as effective, and often the only affordable option for people managing chronic conditions like high blood pressure, diabetes, or thyroid disease. But getting them has always been a hassle. You need a prescription, a trip to the pharmacy, a wait time, and then you hope the insurance didn’t flip the script last minute.
Digital pharmacies flipped that model. Instead of waiting 48 hours for a prescription to be filled, platforms like Truepill and CVS Health now deliver generics in under 5.2 hours-same-day, sometimes even same-hour. How? They use AI to predict demand. If flu season hits Florida, the system automatically boosts stock of generic oseltamivir in regional fulfillment centers. If a patient in rural Montana refills their metformin every 30 days, the system schedules it before they even think about it.
This isn’t magic. It’s data. AI models track historical refill patterns, local outbreak trends, even weather patterns that affect chronic illness flare-ups. The accuracy? 89.7%, according to Deloitte’s 2024 Pharmacy Technology Benchmarking Report. That’s why digital platforms now handle over 10,000 prescriptions daily. And it’s why 78.4% of users report better adherence to their meds.
What’s Actually Changing in Delivery Systems
Modern digital pharmacy delivery isn’t just a website that ships pills. It’s a full-stack system connecting telehealth visits, insurance verification, AI-driven substitution, and automated fulfillment-all in real time.
Here’s how it works: You hop on a telehealth app, talk to a provider about your high cholesterol. They write a prescription for atorvastatin. That prescription goes straight into the pharmacy’s system. The AI checks your insurance, compares generic alternatives, and picks the one covered under your plan. It flags any potential issues-like a previous allergic reaction to a filler in a certain generic version. Then it routes the order to the nearest fulfillment center. Your meds are packed, labeled, and out the door within 90 minutes.
Behind the scenes, it’s all API-driven. Platforms integrate with Epic and Cerner EHRs, insurance clearinghouses like Change Healthcare, and smart pill dispensers that beep when it’s time to take your meds. The result? A 40% drop in processing time and a 92.3% order accuracy rate-compared to 87.6% in traditional pharmacies.
And the delivery? It’s not FedEx. It’s localized. Companies like Honeybee Health and Blink Health use micro-fulfillment centers in urban hubs and regional distribution nodes in rural areas. In cities, delivery takes 12 hours. In the Midwest or Appalachia, it’s 38 hours-but still faster than driving 60 miles to the nearest pharmacy.
Cost Savings You Can Actually See
Price transparency is the biggest win for patients. GoodRx’s 2024 report shows digital platforms save users 22.7% on average for generic medications compared to retail pharmacies. For someone on a $150/month med like levothyroxine, that’s $34 saved every 30 days. Add in no gas, no parking, no time off work, and you’re saving $17.30 per prescription in indirect costs-especially huge for rural patients.
But here’s the catch: not all savings are equal. Some platforms auto-substitute generics based on insurance formularies, not clinical need. One Reddit user, PharmaPatient87, shared how they got a generic version their insurance covered-but it had a different inactive ingredient that caused stomach issues. They lost $83 a month in savings because they had to switch back. Insurance coordination issues are the #1 complaint in negative reviews, mentioned in 41.3% of them.
Platforms are improving. CVS Health’s SmartDUR™ system, launching in late 2024, uses AI to compare therapeutic equivalence between generics-not just price. It flags when a cheaper version might not work for someone with kidney disease or a history of adverse reactions. That’s the future: savings without trade-offs.

The Human Factor: When Tech Falls Short
AI is great at predicting demand and matching prices. But it’s not great at listening. That’s where digital pharmacies still struggle.
Only 43% of digital platforms offer comprehensive medication therapy management (MTM)-the kind of counseling you get in a brick-and-mortar pharmacy where the pharmacist asks how you’re feeling, checks for side effects, and adjusts timing. In traditional pharmacies, 89% do. That gap shows in patient feedback. On Trustpilot, 37.8% of negative reviews mention “lack of personalized counseling.”
And seniors? They’re being left behind. AARP’s 2023 survey found 24% of people over 65 struggle with digital pharmacy apps. They don’t know how to upload a prescription photo. They get confused by pop-ups about insurance. One 71-year-old in Ohio told a local news station she had to call her grandson three times just to refill her metoprolol.
Some companies are responding. Blink Health now offers a free phone-line pharmacy service. CVS lets you schedule a video call with a pharmacist after ordering. But these are add-ons, not standards. The real fix? Designing interfaces for older users from day one-not tacking on help after the fact.
Regulation Is Catching Up-Slowly
Here’s the messy part: digital pharmacy laws vary by state. In 28 states, the pharmacist filling your order must be licensed in your state. That means if you live in Texas and order from a platform based in California, they can’t legally ship your meds unless they have a Texas-licensed pharmacist on staff. That slows down expansion.
And then there’s the issue of generic substitution. The FDA’s 2023 Digital Health Innovation Action Plan set new standards, but 17 states have passed their own laws about when and how generics can be swapped. Some require pharmacist approval. Others let the AI decide. That’s dangerous. In 2023, the FDA issued a safety alert after one platform auto-substituted a different levothyroxine brand, leading to incorrect dosing for 217 patients.
Dr. Michael Cohen of ISMP warns: “Automation without human oversight creates blind spots.” Pharmacists don’t just count pills-they know which generic version has a slower release, which one triggers a rash in certain patients, which one interacts with a patient’s coffee habit. AI can’t learn that unless it’s trained on real-world data-and even then, it needs a human to double-check.
Who’s Winning the Digital Pharmacy Race?
By 2024, three models dominate:
- Integrated Retailers: CVS Health (28.4% market share), Walgreens. They’ve got stores, insurance deals, and EHR access.
- Pure Digital Players: Ro, Honeybee Health, Truepill. They’re lean, fast, and tech-first.
- Specialty Platforms: Blink Health focuses on price transparency. Amazon Pharmacy uses Prime logistics.
CVS leads because they combine physical presence with digital tools. You can order online, pick up at the store, or get it delivered. Ro wins with sleek design and telehealth bundling. But the real innovation is happening at the edges. Blink Health shows you the exact price before you order-no surprises. Honeybee Health lets you chat with a pharmacist before you pay.
Market share is shifting fast. Digital channels captured 31.2% of generic medication dispensing in 2024-up from 18.7% in 2022. By 2027, Deloitte predicts that number will hit 47.8%.
The Future: Personalized Generics and AI Pharmacists
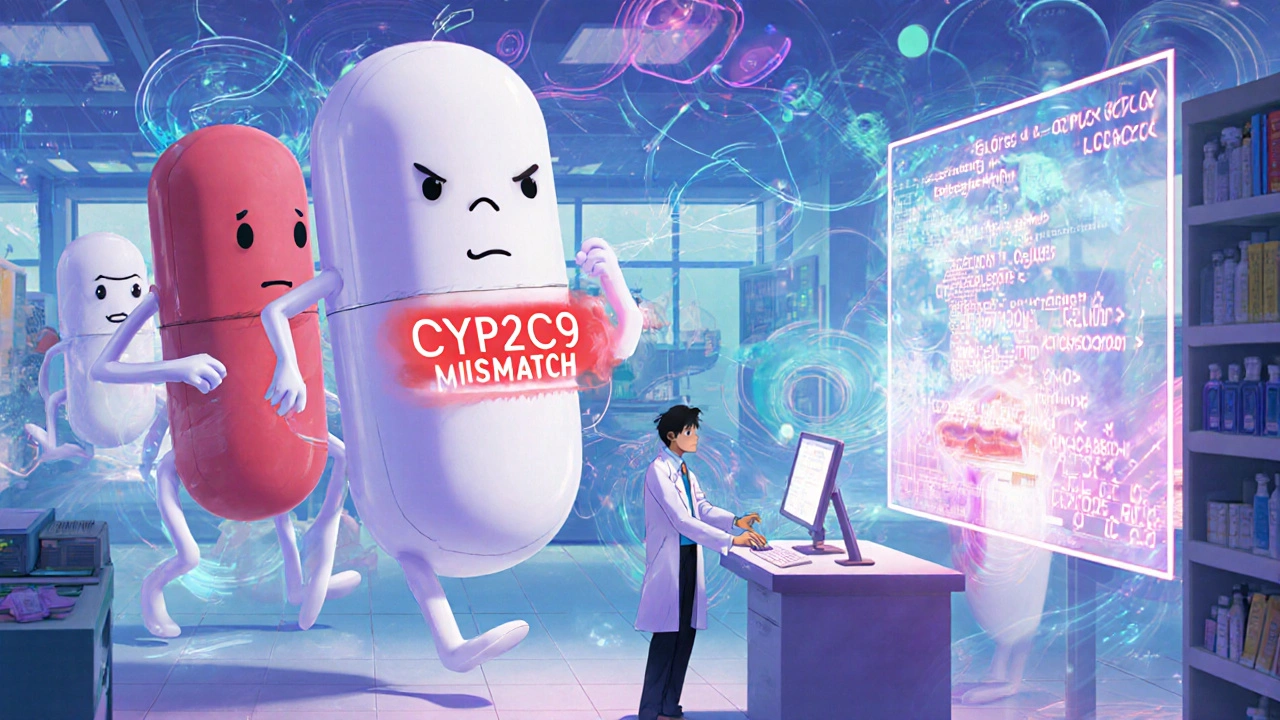
The next leap isn’t faster delivery-it’s smarter selection. By 2026, PwC predicts 74% of digital platforms will use pharmacogenomic data to choose generics. That means your meds won’t just be “generic atorvastatin.” They’ll be “generic atorvastatin that matches your CYP2C9 gene variant,” reducing side effects and boosting effectiveness.
Pharmacy schools are already adapting. The University of Florida launched mandatory AI literacy training for all new pharmacy students in fall 2024. They’re learning how to audit AI substitution algorithms, spot biased data, and override automated decisions when needed.
AI will handle 52.3% of prior authorization requests by 2025, cutting approval time from 72 hours to under 4. That’s huge for patients on tight budgets. But it also means pharmacists need to shift from pill counters to data interpreters.
And yes, risks remain. Cybersecurity is a nightmare. In 2023, 378 pharmacy data breaches exposed 14.2 million patients. Digital platforms made up 63% of those. Encryption (AES-256) is standard, but human error isn’t. A misconfigured server, a phishing email, a weak password-those are still the biggest threats.
What This Means for You
If you take generics, you’re already in the middle of this shift. Here’s what to do:
- Compare prices before you order. Use GoodRx or SingleCare to see what the same generic costs across platforms.
- Check if the platform offers pharmacist chat. Don’t settle for auto-fill. You deserve to ask questions.
- Know your generics. If you’ve had side effects with one brand, note the manufacturer. Ask for that specific version.
- Use reminders. If your platform offers smart pill dispensers or text alerts, turn them on. Adherence improves by 28% with them.
- Speak up. If you’re over 65 and struggling with the app, call customer service. Demand phone support. Your voice pushes change.
Digital pharmacy isn’t perfect. But it’s better than the old system. It’s faster, cheaper, and more accessible. The goal isn’t to replace your pharmacist-it’s to give them the tools to do more, better, and reach more people. That’s the future. And it’s already here.







Digital pharmacy isn’t just a logistical upgrade-it’s a redefinition of care delivery. The AI-driven refill systems are astonishingly accurate, but what’s rarely discussed is how they redistribute labor. Pharmacists are no longer bottlenecks; they’re clinical analysts. The same person who used to count pills now interprets pharmacogenomic flags and overrides algorithmic substitutions. That’s a massive upskilling curve, and most training programs haven’t caught up. We’re creating a new class of healthcare professionals without the curriculum to support them.
And let’s not romanticize the delivery speed. A 5.2-hour turnaround means nothing if the patient can’t open the app, doesn’t understand the difference between levothyroxine brands, or can’t afford the copay even after the 22.7% discount. Convenience without accessibility is just another form of exclusion.
The real win? The data. Every refill, every skipped dose, every side effect logged creates a feedback loop that improves outcomes. But who owns that data? The insurer? The platform? The patient? We’re building a healthcare infrastructure on data we don’t legally or ethically know how to steward.
And yes, seniors are being left behind-but not because they’re technologically inept. Because the interfaces were designed for 25-year-olds who scroll through TikTok between sips of cold brew. Design for the oldest first, and you design for everyone.
The FDA’s 2023 alert on levothyroxine substitution? That wasn’t a glitch. It was a symptom. We automated the wrong part of the process. We optimized for cost and speed, not safety. AI doesn’t know that one patient’s rash isn’t from the drug-it’s from the dye in the capsule that their body has rejected since 2012. Only a human remembers that.
We need pharmacists as gatekeepers of nuance, not just validators of algorithms. The future isn’t AI replacing pharmacists. It’s pharmacists teaching AI to be less dumb.
Let’s cut through the Silicon Valley fluff. Digital pharmacy is just another capitalist hack to extract value from chronic illness. Yes, it’s faster. Yes, it’s cheaper. But at what cost? The erosion of the pharmacist-patient relationship isn’t a side effect-it’s the business model. Why train a human to listen when an algorithm can auto-substitute and upsell a generic with a 3% higher margin? The 78.4% adherence rate? That’s not because patients feel cared for-it’s because they’re trapped in a system that auto-replenishes their meds before they can say no.
And don’t get me started on the ‘personalized generics’ hype. Pharmacogenomics is still in its infancy. We’re not predicting drug response-we’re gambling with SNPs and hoping the statistical noise doesn’t kill someone. The University of Florida’s AI literacy program? Cute. But you can’t teach a pharmacist to audit bias in a model trained on data from 90% white, middle-class patients while ignoring rural Black populations with higher rates of CYP2C19 polymorphisms.
Amazon Pharmacy? They’re not here to save lives. They’re here to lock you into Prime. CVS? They’re using digital pharmacy to extend their insurance monopoly. This isn’t innovation-it’s consolidation wrapped in a white coat.
And let’s not forget: 63% of data breaches came from digital platforms. Your blood pressure meds are now a target for ransomware. The system isn’t secure. It’s just invisible until it’s too late.
Real progress? Universal healthcare with free pharmacy access. Not a better app.
I’ve been using Blink Health for my metformin for two years now. No more driving 45 minutes to the pharmacy, no more insurance drama. I get my meds in 36 hours even in rural Tennessee. The price is always listed upfront. I know exactly what I’m paying. It’s been life-changing.
But I’ll be honest-I still call the phone line when I have questions. The chat with the pharmacist before I order? That’s the real magic. Not the AI. Not the speed. The person on the other end who remembers I’m on warfarin and asks if I’ve been eating more kale.
They don’t need to replace pharmacists. They just need to let them talk to patients. That’s it.
Also-yes, seniors struggle. But give them a printed QR code with a toll-free number taped to their fridge. Problem solved. Tech isn’t the enemy. Poor design is.
Oh wow, so now we’re celebrating automation that accidentally dosed 217 people because some algorithm thought ‘generic levothyroxine’ meant ‘all levothyroxine are the same’? Brilliant. Truly visionary. The FDA had to issue a safety alert because someone thought ‘efficacy’ was just a marketing buzzword.
And you call this progress? I call it negligence dressed in a hoodie. Next they’ll automate insulin dosing and blame the patient for ‘non-adherence’ when the AI gave them 20 units instead of 2.
Also, ‘smart pill dispensers’? My grandma’s pillbox beeps. That’s not innovation. That’s a toaster with Bluetooth. Stop pretending tech fixes human problems. It just makes them louder.
As someone from India where pharmacy access is a daily struggle, I can’t tell you how moved I am by this. Here, people walk 10 km to get insulin because the nearest clinic is in the next town. The idea that someone in Montana can get metformin in 38 hours? That’s not convenience-that’s justice.
Yes, the tech isn’t perfect. Yes, seniors need better interfaces. But let’s not let the perfect be the enemy of the life-saving. In rural India, we don’t have AI-but we do have WhatsApp groups where community health workers coordinate generic drug orders. We’re doing it with low-tech, high-heart solutions.
Maybe the future isn’t just about algorithms. Maybe it’s about adapting what works-whether it’s AI in Ohio or a grandmother with a phone in Bihar.
Also, I love how you mentioned pharmacogenomics. That’s the future. My cousin has a CYP2D6 mutation and gets sick on standard antidepressants. Imagine if her meds were chosen based on her DNA, not her insurance formulary. That’s real innovation.
This is exactly the kind of progress we need-thoughtful, data-driven, and centered on human outcomes. The fact that digital platforms are now reducing processing time by 40% while improving accuracy to 92.3% is nothing short of revolutionary. And the emphasis on therapeutic equivalence over price? That’s the kind of ethical innovation that should be the industry standard, not the exception.
I especially appreciate the call to action for users: know your generics, ask questions, demand phone support. Empowerment isn’t just a buzzword-it’s the foundation of sustainable healthcare. When patients are informed, they become partners, not passive recipients.
And to those who fear AI replacing pharmacists? That’s a misunderstanding. AI isn’t replacing the human-it’s freeing the human from repetitive tasks so they can do what only humans can: listen, adapt, and care. That’s not a threat. That’s evolution.
Let’s keep pushing for design that includes elders, for regulation that prioritizes safety over speed, and for platforms that treat medication not as a commodity, but as a lifeline.
Thank you for writing this. It’s hopeful without being naive.
I work in a rural clinic in West Virginia. We have one pharmacy in a 60-mile radius. It’s closed on Sundays. People skip doses because they can’t get there. I’ve seen diabetic patients go without insulin for a week because they didn’t have gas money.
Digital pharmacy isn’t a luxury here. It’s survival.
Yes, the app is clunky. Yes, some seniors can’t use it. But we’ve started printing QR codes with a toll-free number and handing them out with prescriptions. We train the kids to help their grandparents. It’s not perfect, but it’s working.
One woman, 74, got her blood pressure meds delivered last week. She cried. Said she hadn’t left the house in three weeks. That’s not a metric. That’s a human being.
We need more of this. Not less.
And the AI? It doesn’t need to be perfect. It just needs to be better than the alternative. And right now, the alternative is people dying because they can’t get to a pharmacy.
Deloitte’s 47.8% projection is statistically sound but ethically naive. The model assumes universal digital literacy, perfect insurance integration, and zero regulatory friction. Reality? 28 states require state-licensed pharmacists. Only 12% of digital platforms comply fully. The 31.2% market share in 2024 is inflated by urban centers. In Appalachia, the number is 8%.
The 89.7% AI prediction accuracy? That’s on historical refill data. What happens when a pandemic hits? When supply chains collapse? When a new generic is recalled? The model doesn’t account for chaos. It assumes equilibrium.
And the pharmacogenomic push? We’re talking about sequencing genes for $10 generics. The marginal benefit is negligible compared to the cost of implementation. Meanwhile, 14 million patient records were breached last year. That’s not a bug. It’s a feature of a system optimized for profit, not safety.
Let’s stop calling this innovation. It’s optimization. And optimization without ethics is just exploitation with a better UI.
I just want to say-thank you. This article made me cry. Not because it’s perfect, but because it’s real. I’m a single mom on SSI. My levothyroxine used to cost $120 a month. Now I get it for $38 through Honeybee. I don’t have to choose between meds and groceries anymore.
Yes, I had to call five times to get my first order right. Yes, I didn’t understand the difference between the two generic brands. But the pharmacist on the phone? She didn’t judge me. She explained it like I was five. That’s the part they don’t talk about.
It’s not about the AI. It’s about the person behind it.
Don’t take that away. Just make it easier to find.
I’m a pharmacy student. We’re learning AI tools in class now. We’re taught to question the algorithm, not trust it. One professor said, ‘If the AI says give patient A this generic, ask why. Then ask what’s different about patient B.’
That’s the future. Not robots replacing humans. Humans using robots to be better humans.
Also, I love that the article mentions GoodRx. I showed my grandma how to use it. She saved $40 on her statin. She said, ‘I didn’t know I could do that.’
Simple tools. Big impact.
...I just... I mean... the data... the... 92.3% accuracy... and the 40% reduction... but... what about the 378 breaches? And the 217 patients? And the fact that... I mean... are we sure? Are we really sure? I just... I don’t know... I think maybe... maybe we should slow down? Just a little? Just to be safe? I mean... I’m not saying no... I’m just saying... maybe...?
Response to Olivia: You’re right. The human element is everything. But here’s the catch: the system isn’t designed to scale human interaction. It’s designed to minimize it. That’s why phone support is an ‘add-on,’ not a feature. That’s why video calls cost extra. That’s why MTM is optional.
True innovation would be mandatory, free, 24/7 pharmacist access built into every digital pharmacy platform. Not as a perk. As a requirement. Like seatbelts. Like fire exits.
Because if we’re going to automate the dispensing, we owe patients the human backup. Not as a bonus. As a duty.