Chronic Alcohol Use Disorder isn’t just about drinking too much. It’s a medical condition where your brain and body become wired to need alcohol-even when it’s destroying your health, relationships, or job. You might not even realize it’s happening until you’re stuck in a cycle of drinking to feel normal, then feeling worse when you stop. The truth? This isn’t a lack of willpower. It’s a brain disease, and like any other chronic illness, it needs real treatment-not judgment.
What Happens to Your Body When You Drink Too Much for Too Long
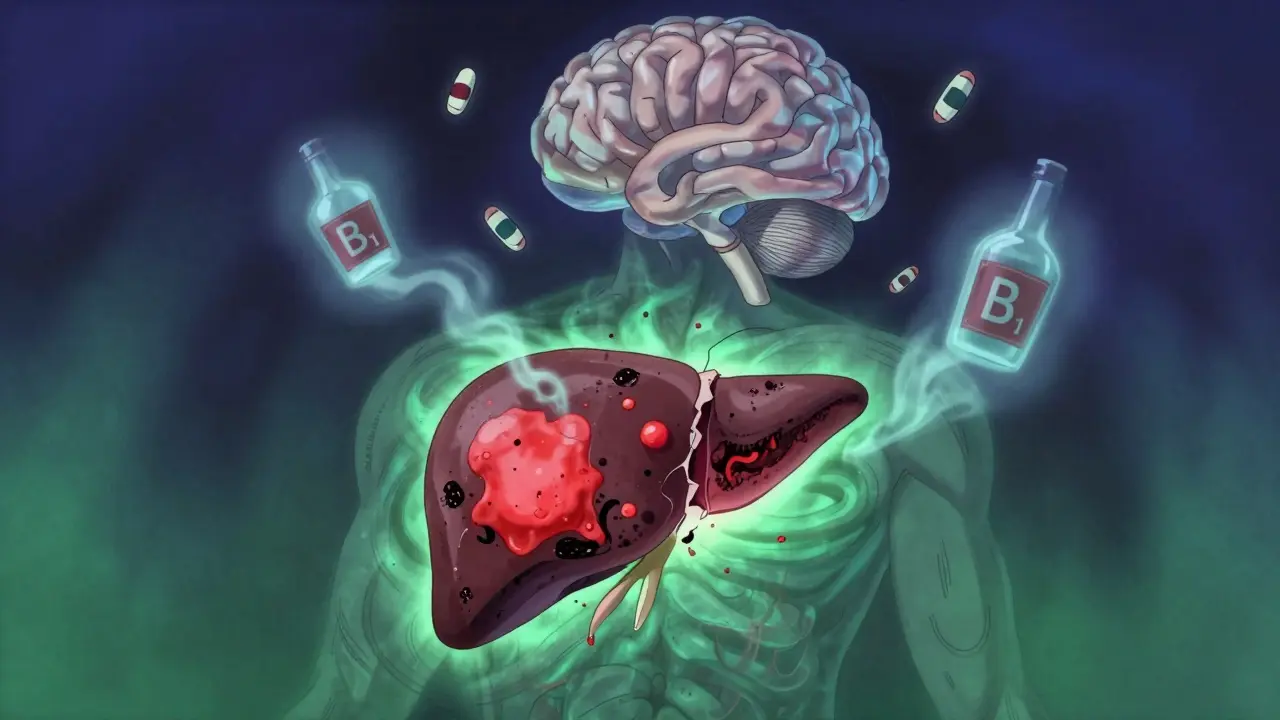
Your body doesn’t handle alcohol the way it handles water or food. Every time you drink, your liver has to break it down. But if you’re drinking heavily every day, that liver gets overwhelmed. Over time, fat builds up in liver cells-this is called fatty liver. It affects nearly 90% of heavy drinkers. At this stage, you might feel fine. No pain. No symptoms. But the damage is already there. If drinking continues, the next stage is alcoholic hepatitis. Your liver becomes inflamed, cells start dying, and you might begin to feel nausea, fever, or jaundice-yellowing of the skin and eyes. This isn’t just uncomfortable. It’s dangerous. Left unchecked, it leads to cirrhosis. That’s when healthy liver tissue turns into scar tissue. Scar tissue doesn’t work. Once cirrhosis sets in, your liver can’t filter toxins, make proteins, or store energy like it should. Some damage can reverse if you stop drinking completely. But not all of it. The longer you wait, the less chance you have of full recovery. It’s not just your liver. Alcohol hits your brain hard. It slows down your nervous system, which is why you feel relaxed at first. But over time, it damages nerve cells. You might start having trouble remembering things, thinking clearly, or even walking straight. Numbness or burning in your hands and feet? That’s nerve damage. Long-term drinkers are also at higher risk for dementia and memory loss. Thiamine (vitamin B1) deficiency is common-up to 80% of people with AUD are deficient. Without enough thiamine, your brain can develop Wernicke’s encephalopathy: confusion, unsteady gait, and eye movement problems. Left untreated, it can lead to permanent brain damage. Your heart takes a beating too. Heavy drinking raises blood pressure, causes irregular heart rhythms like atrial fibrillation, and increases your risk of heart attack and stroke. Studies show heavy drinkers have a 34% higher risk of stroke and a 40% higher risk of atrial fibrillation. Even if you don’t feel it, your heart is working harder than it should. And then there’s cancer. Alcohol is a known carcinogen. It raises your risk for mouth, throat, esophagus, liver, breast, and bowel cancers. For example, heavy drinkers are five times more likely to get mouth cancer. Just one drink a day increases breast cancer risk by 12%. There’s no safe level when it comes to cancer risk.Alcohol Doesn’t Just Hurt Your Body-It Breaks Your Life
The physical damage is bad enough. But the ripple effects are worse. People with chronic alcohol use disorder often lose jobs, relationships, and homes. Depression and anxiety don’t just happen alongside AUD-they’re fueled by it. Alcohol messes with serotonin and dopamine, the chemicals that regulate mood. You might start drinking to feel better, but over time, you need more just to feel normal. That’s the trap. Your immune system weakens. You’re 2.7 times more likely to get pneumonia. Simple infections become life-threatening. You’re more likely to fall, get injured, or be involved in a car crash. In the U.S., alcohol is involved in 29% of all traffic deaths. It’s also linked to domestic violence, criminal behavior, and suicide. And the cost? In 2010, excessive alcohol use cost the U.S. $249 billion. Most of that came from lost productivity, healthcare, and criminal justice expenses. Globally, alcohol causes 3 million deaths every year. That’s more than HIV, tuberculosis, or road injuries.Treatment Isn’t One-Size-Fits-All
The good news? AUD is treatable. And recovery doesn’t mean you have to hit rock bottom. You don’t need to be homeless or in a hospital to start getting help. Treatment works best when it’s personalized. First step for many: detox. If you’ve been drinking heavily for months or years, stopping cold turkey can be deadly. Withdrawal can cause seizures, hallucinations, or delirium tremens-a life-threatening condition with high fever, confusion, and rapid heartbeat. That’s why medically supervised detox is critical. Doctors can give you medications like benzodiazepines to safely manage withdrawal symptoms. After detox, the real work begins. Three FDA-approved medications help with long-term recovery:- Naltrexone blocks the pleasurable effects of alcohol. If you drink while on it, you won’t get the same high. That reduces cravings over time.
- Acamprosate helps your brain chemistry return to normal. It’s especially helpful for people who’ve been sober for a while but still feel anxious or restless.
- Disulfiram makes you sick if you drink. It causes nausea, vomiting, and flushing. It’s not for everyone, but for some, the fear of feeling awful is enough to keep them from drinking.

Therapy Changes the Way You Think
Medications help with the body. Therapy helps with the mind. Cognitive Behavioral Therapy (CBT) is one of the most effective. It teaches you to spot triggers-like stress, certain people, or places-and replace drinking with healthier responses. Studies show CBT reduces heavy drinking days by 60%. Motivational Enhancement Therapy (MET) helps you find your own reasons to quit. It doesn’t push you. It helps you talk through your doubts and build your own motivation. Support groups like Alcoholics Anonymous (AA) have helped millions since 1935. The 12-step model isn’t for everyone, but the community aspect matters. People who stay connected to support groups are more likely to stay sober. AA reports about 27% of members stay abstinent after one year. That’s not perfect, but it’s better than going it alone.New Treatments Are Changing the Game
Science is catching up. In 2022, a study in JAMA Psychiatry found that transcranial magnetic stimulation (TMS)-a non-invasive brain stimulation technique-led to 50% abstinence rates in people with severe AUD. It targets areas of the brain involved in cravings. Another breakthrough is the reSET app, an FDA-approved digital therapy tool. In clinical trials, people using reSET were nearly twice as likely to stay sober compared to those who didn’t. The MATTERS study showed something powerful: combining medication with therapy increases abstinence rates by 24% compared to either one alone. That’s the new standard. No single treatment works for everyone. But together, they create a safety net.
Recovery Is Possible-Even After Years
Some people believe that if you’ve been drinking for decades, it’s too late. That’s a myth. Even with cirrhosis, stopping alcohol can stop further damage. Some liver function can improve. Your brain can heal. Your relationships can mend. You can get your life back. The biggest barrier isn’t the addiction. It’s the shame. Too many people think they need to be ‘ready’ or ‘hit rock bottom’ before they deserve help. But recovery doesn’t wait. The earlier you act, the more you save-your liver, your mind, your family, your future. You don’t need to be perfect. You don’t need to quit overnight. You just need to start. One day at a time. One step. One call to a doctor. One therapy session. One meeting. That’s how it begins.What to Do If You or Someone You Know Is Struggling
If you’re reading this and thinking, ‘This sounds like me,’ here’s what to do next:- Make an appointment with your doctor. Ask for a screening for alcohol use disorder. It’s a simple checklist-no judgment.
- Call a local addiction service. In the UK, you can contact NHS Alcohol Services or Alcoholics Anonymous. They’ll connect you to free or low-cost support.
- Don’t try to quit alone if you’ve been drinking heavily. Detox can be dangerous without medical help.
- Consider medication. Ask your doctor if naltrexone or acamprosate could help.
- Find a support group-even if you’re skeptical. One meeting might change everything.
If you’re worried about someone else, don’t wait for them to ‘ask for help.’ Talk to them calmly. Say: ‘I care about you, and I’ve noticed you’ve been drinking more. I’m worried. Let’s talk to someone together.’
Is alcohol use disorder the same as alcoholism?
Yes. Alcoholism is the older, informal term. The medical term now is Alcohol Use Disorder (AUD). It’s diagnosed as mild, moderate, or severe based on how many symptoms you have. Alcoholism usually refers to the severe form, but AUD covers the full spectrum-from occasional binge drinking to daily dependence.
Can you recover from liver damage caused by alcohol?
It depends on how far the damage has gone. Fatty liver and early alcoholic hepatitis can reverse if you stop drinking completely. Cirrhosis is more serious-scarring is permanent. But even with cirrhosis, stopping alcohol can stop further damage and improve survival. Some people live for decades after diagnosis if they stay sober.
How long does alcohol withdrawal last?
Withdrawal symptoms usually start 6-12 hours after your last drink. Peak symptoms happen in 24-72 hours. Most physical symptoms like shaking, nausea, and sweating fade within a week. But sleep problems, anxiety, and cravings can last weeks or months. That’s why ongoing support is essential. Medical detox helps manage the worst of it safely.
Do medications for AUD just replace one addiction with another?
No. Medications like naltrexone and acamprosate don’t create a high or dependence. They help restore brain chemistry and reduce cravings so you can focus on therapy and rebuilding your life. Think of them like insulin for diabetes-they treat the underlying imbalance, not just the symptoms.
Is it safe to quit drinking cold turkey?
If you’ve been drinking heavily for months or years, quitting cold turkey can be life-threatening. Seizures and delirium tremens can happen without medical supervision. Always talk to a doctor before stopping. They can help you detox safely with medication and monitoring.
Can I still drink socially after treatment?
For most people with chronic AUD, the answer is no. Alcohol use disorder rewires the brain. Even one drink can trigger a full relapse. Recovery usually means complete abstinence. Some people try controlled drinking, but the risk of relapse is very high. Abstinence is the safest path to long-term health.







Let's be clear: AUD is a neuroadaptive disorder characterized by dysregulation of the mesolimbic dopamine pathway, with concurrent downregulation of prefrontal cortical inhibitory control mechanisms. The GABA-glutamate imbalance is profound, and chronic ethanol exposure induces epigenetic modifications in the nucleus accumbens that perpetuate craving cycles. This isn't moral failure-it's a neurobiological pathology requiring pharmacological intervention and neurocognitive rehabilitation. The literature is unequivocal: abstinence + MAT + CBT yields the highest sustained remission rates, particularly when targeting executive function deficits.
Furthermore, the hepatic metabolism of ethanol via ADH and CYP2E1 generates acetaldehyde and ROS, which trigger mitochondrial dysfunction and Kupffer cell activation. Cirrhosis isn't just fibrosis-it's a dysregulated wound-healing response driven by hepatic stellate cell transdifferentiation. Early intervention can halt progression, but only if we stop framing this as a behavioral issue and start treating it like we treat Parkinson's or epilepsy.
And yes, naltrexone is a mu-opioid receptor antagonist that reduces reinforcement, but its efficacy is amplified when combined with fMRI-guided cue-exposure therapy. The 2022 JAMA Psychiatry TMS trial? Groundbreaking. It modulates the dorsolateral prefrontal cortex, disrupting craving circuitry without systemic side effects. This is medicine. Not willpower.
Stop romanticizing 'rock bottom.' Recovery is neuroplasticity in action. You don't need to lose everything to deserve help-you just need to be alive.
Also, 'alcoholism' is an outdated term. DSM-5 uses AUD because it's dimensional, not categorical. The spectrum matters.
Thiamine deficiency? That's Wernicke-Korsakoff syndrome. It's not 'just memory loss.' It's irreversible neurodegeneration if untreated. Screen everyone with suspected AUD for B1 levels. Immediately.
And for the love of science, stop telling people they can 'drink in moderation' after AUD. That's like telling a diabetic they can have one donut. The brain doesn't forget the reward pathway.
It's not about being 'strong.' It's about neurobiology. We treat other brain diseases with medication. Why not this one?
OMG YES!! THIS!! 🙌🔥 I’ve been screaming this from the rooftops for YEARS-alcohol isn’t a ‘bad habit,’ it’s a BRAIN DISEASE!! I’m so tired of people saying ‘just quit’ like it’s choosing between coffee and tea!! 🤦♀️
My cousin was a ‘functioning alcoholic’ for 15 years-held a job, paid taxes, looked fine… until one day she couldn’t walk straight. Turns out? Her liver was basically a brick. Now she’s on naltrexone, goes to therapy twice a week, and actually smiles again. 💛
And TMS?! That’s like a brain reset button!! I’m telling my therapist RIGHT NOW!!
Also-STOP TELLING PEOPLE TO ‘DRINK RESPONSIBLY.’ If you’ve got AUD, that’s like handing a heroin addict a tiny dose and saying ‘be cool.’ NO. JUST NO.
YOU AREN’T WEAK. YOU’RE ILL. AND YOU DESERVE HELP. NOT JUDGMENT. 💪❤️
It's important to contextualize the global burden of alcohol use disorder within the framework of public health epidemiology. While the U.S. data is compelling, the World Health Organization reports that low- and middle-income countries bear nearly 70% of alcohol-attributable deaths, often with minimal access to detox facilities or FDA-approved medications. In Nigeria, for instance, traditional healers and faith-based interventions remain primary points of care, despite lacking evidence-based protocols.
The socioeconomic cost of AUD-$249 billion in the U.S. alone-is staggering, but the human cost is even more profound: fractured families, lost generations of productivity, and intergenerational trauma. The stigma surrounding AUD in many cultures prevents early intervention, particularly among men who are socialized to equate vulnerability with weakness.
Moreover, the pharmacological tools available-naltrexone, acamprosate, disulfiram-are underutilized due to provider ignorance, insurance barriers, and the persistent myth that recovery must be ‘spiritual’ or ‘willpower-driven.’ Meanwhile, digital therapeutics like reSET are proving effective, especially among younger populations who are more receptive to app-based interventions.
We need a paradigm shift: AUD is not a moral failing. It is a chronic relapsing condition, akin to asthma or hypertension, requiring long-term management, not punishment. Screening should be routine in primary care, just like cholesterol checks. And insurance companies must cover MAT as standard of care-not as an afterthought.
Recovery is possible. But only if society stops treating it like a crime and starts treating it like a health crisis.
Ohhhhh, so now we’re calling it a ‘brain disease’? 😏 Like, wow, what a revelation. I guess all those people who just ‘lose control’ aren’t just weak? They’re… neurologically impaired? 🤯
Meanwhile, my neighbor drinks a six-pack every night and still coaches his kid’s soccer team. So what’s the real difference? Is it the number of drinks? Or is it that some people just don’t have the spine to admit they’re a mess?
And don’t get me started on ‘medications.’ Naltrexone? So now we’re drugging people so they can’t enjoy a beer? 😭
Here’s a radical idea: maybe people should just… stop. Like, in 1950, nobody needed a pill to quit smoking. People just quit. Why? Because they WANTED to. Not because some doctor told them their brain was ‘broken.’
Also, TMS? Sounds like a sci-fi movie. Next thing you know, they’ll be implanting chips to make you not want alcohol. 🤖
Stop infantilizing adults. You’re not sick. You’re selfish. And you’re using ‘brain disease’ as an excuse to avoid accountability. 😒
It is imperative to underscore that the medicalization of alcohol use disorder, while well-intentioned, inadvertently erodes personal responsibility-a foundational pillar of ethical autonomy. The notion that an individual’s behavioral choices can be entirely subsumed under a neurobiological framework is not only scientifically reductive but morally perilous.
One may posit that the dopaminergic dysregulation is real; however, to absolve the individual of agency is to dismantle the very structure of moral accountability. If one’s actions are determined by neural pathways, then no act-be it virtuous or heinous-is truly one’s own.
Moreover, the proliferation of pharmacological interventions risks creating a dependency on external chemical solutions, rather than cultivating the internal fortitude required for genuine transformation.
Consider the cultural implications: if we teach generations that their vices are illnesses, we foster a society of perpetual victimhood. The 12-step model, flawed as it may be, at least demands acknowledgment of powerlessness-whereas the modern paradigm seeks to outsource willpower to pharmaceuticals.
And yet, we must not overlook the devastating social consequences: the erosion of familial bonds, the normalization of intoxication, the commodification of recovery as a profitable industry.
True healing requires confrontation, not pharmacology. Courage, not chemically induced indifference.
One cannot heal by numbing the pain. One must face it. With eyes open. Without a pill.
Let us not mistake compassion for coddling.
From the perspective of a Nigerian who grew up in a culture where alcohol is both a social lubricant and a spiritual offering, I see this as a global tragedy wrapped in cultural misunderstanding.
In my village, elders would drink palm wine during ceremonies-not every day, not to escape, but to honor ancestors. But now, with urbanization and the flood of cheap industrial alcohol, we’re seeing a silent epidemic among young men who drink to numb trauma, unemployment, or the weight of broken dreams.
Here’s the truth: in many African communities, we don’t have access to naltrexone or TMS. We have community circles. We have church prayers. We have grandmothers who sit with you until you cry. We have silence that says, ‘I see you, and I’m not leaving.’
Western medicine talks about ‘brain chemistry.’ We talk about ‘soul hunger.’
Maybe the answer isn’t just pills or apps. Maybe it’s reweaving the fabric of belonging. Maybe recovery isn’t about stopping drinking-it’s about finding something worth living for.
I’ve seen men sober for 12 years because they started teaching kids to play football. Not because of a doctor. Because of a child who looked up to them.
Let’s not lose the human part while we’re busy mapping the neurons.
The assertion that alcohol use disorder constitutes a ‘brain disease’ is a dangerous oversimplification that ignores the role of volition, character, and personal responsibility. While neurobiological changes occur in chronic users, these are not unique to alcohol; they are also observed in individuals addicted to gambling, pornography, and social media. To classify AUD as a disease on par with Alzheimer’s or multiple sclerosis is to equate pathology with choice, which is both scientifically inaccurate and ethically indefensible.
Furthermore, the widespread promotion of pharmacological interventions such as naltrexone and acamprosate reflects a broader trend in modern medicine: the commodification of human suffering through pharmaceutical solutions. These drugs do not restore neural homeostasis-they merely suppress symptoms while leaving the underlying behavioral and psychological drivers unaddressed.
There is no empirical evidence to support the claim that medication alone leads to sustained recovery. Long-term abstinence correlates strongly with psychosocial support, spiritual awakening, and personal accountability-not pharmacological suppression.
Lastly, the notion that ‘there is no safe level’ of alcohol consumption with respect to cancer risk is misleading. The relative risk increase for breast cancer with one drink per day is 12%, but this translates to a negligible absolute risk increase for most women, particularly when weighed against other lifestyle factors such as obesity, sedentary behavior, and environmental toxins.
Let us not mistake statistical correlation for deterministic causation. Let us not infantilize adults by removing their capacity for self-direction. Recovery is not a medical procedure. It is a moral journey.
I WAS THIS PERSON. I drank 3 bottles of wine a night. For 7 years. I had cirrhosis. I lost my job. My husband left. I was in the hospital with hepatic encephalopathy and they said I had 6 months to live unless I stopped.
So I did. I didn’t want to. I screamed. I cried. I threw things. I begged for one more drink. I hated everyone who told me to ‘just quit.’
Then I got on naltrexone. And I went to therapy. And I found a group of people who didn’t judge me. And I started painting. And now? I’m 3 years sober. My liver’s still scarred. But I’m alive.
And if you’re reading this and you’re still drinking… I’m not saying you’re broken. I’m saying you’re not alone. And you’re worth saving.
Don’t wait for a hospital bed. Don’t wait for your kid to stop looking at you like you’re a ghost.
Call someone. Today. I’ll wait.
❤️
EVERYTHING YOU SAID IS A LIE. 😠
Alcohol isn’t the problem. It’s the government. The pharmaceutical industry. The FDA. They WANT you to think you’re ‘diseased’ so they can sell you pills. Naltrexone? It’s a cover for Big Pharma’s profit margins. They don’t want you cured-they want you on it forever.
And TMS? That’s a mind-control tech from the CIA’s MKUltra program. They’re zapping your brain to make you compliant. Why do you think they call it ‘recovery’? Because they don’t want you to be free. They want you dependent on their system.
Also-why is it always ‘abstinence’? Why can’t we just drink less? Because the AA cult wants you to admit you’re powerless. That’s mind control. That’s cult behavior.
My uncle drank for 40 years. He never went to a meeting. Never took a pill. He just switched to organic wine and now he’s 82 and plays golf every day. So much for ‘no safe level.’
And the cancer stats? Totally cherry-picked. They ignore the French Paradox-people who drink red wine live longer! It’s all propaganda.
Wake up. They’re lying to you. You’re not sick. You’re being manipulated.
Stop trusting doctors. Stop trusting apps. Stop trusting ‘science.’
Drink your wine. Live your life. They can’t control you unless you let them.
🔥
Look, I get why people are mad at the ‘brain disease’ framing. It feels like an excuse. But here’s the thing: it’s not about absolving responsibility-it’s about removing shame. You can be responsible AND sick. Like, I have asthma. I don’t get to blame my lungs. But I still have to use my inhaler and avoid triggers. Same here.
And yes, the meds don’t make you ‘not want’ alcohol. They take the edge off the craving so you can actually do the hard work: therapy, rebuilding trust, learning to sit with discomfort.
And TMS? It’s real. I know someone who did it. He went from 3 drinks a night to zero. Not because he was ‘stronger.’ Because his brain stopped screaming for it.
Also-yes, AA isn’t for everyone. But the fact that 27% stay sober? That’s better than 0%. And if you think ‘spiritual’ means ‘religious,’ you’re wrong. It means ‘connected.’ To people. To purpose.
And no, you don’t have to be a mess to deserve help. You just have to be tired.
And yes-I’ve had a drink after being sober for a year. And I didn’t relapse. Because I had tools. And support. And I didn’t shame myself.
It’s not about perfection. It’s about showing up.
And if you’re still reading this… you’re already trying. That counts.
🙂
I used to work in ER. Saw the same faces every weekend. Same guy. Same broken nose. Same story: ‘I don’t remember.’
One night, a guy came in with a seizure. 42 years old. Hadn’t eaten in 3 days. Smelled like a distillery. He was shaking so bad his teeth chattered. I held his hand while they gave him benzodiazepines. He whispered, ‘I didn’t want to die.’
He didn’t say ‘I’m weak.’ He didn’t say ‘I’m an addict.’ He said ‘I didn’t want to die.’
That’s the moment I stopped seeing ‘alcoholics.’ I started seeing people who were drowning-and nobody had handed them a life preserver.
Medication? Therapy? Support groups? They’re not magic. They’re just tools. Like a cast for a broken leg. You don’t say ‘just walk it off.’ You fix it.
And yeah, some people relapse. So what? They didn’t fail. The system failed them. We didn’t give them enough time. Enough care. Enough love.
Recovery isn’t a finish line. It’s a daily practice. Like brushing your teeth. Or eating vegetables. Or calling your mom.
You don’t have to be perfect. Just present.
And if you’re reading this… you’re already halfway there.
It is lamentable that Western societies have embraced a pathological model of human behavior that undermines the moral fabric of society. In India, we have a long tradition of self-discipline, rooted in ancient philosophies such as Yoga and Ayurveda, which emphasize control over the senses as the highest form of strength. To reduce the willful choice to consume alcohol to a neurological disorder is not only scientifically unsound, but culturally imperialistic.
Alcohol consumption is a choice, and the consequences are the natural result of that choice. To medicalize it is to infantilize the individual and absolve them of the dignity of personal accountability.
Moreover, the promotion of pharmaceutical interventions is a form of cultural colonization-imposing foreign, profit-driven models of healing upon societies that have thrived for millennia without them.
Let us not forget: the most powerful cure for addiction has always been discipline, community, and spiritual purpose-not chemical suppression.
Do not mistake compassion for weakness. Do not mistake recovery for dependency on state-sanctioned drugs.
True healing comes from within. Not from a pill. Not from a machine. Not from an app.
It comes from the soul.
Okay, but have you ever met someone who quit drinking and became… *better*? Like, not just sober-actually happier, calmer, funnier? My cousin did. She used to cry in the shower every night. Now she runs marathons and makes pottery. And she says the best part? She doesn’t need alcohol to feel anything anymore.
Also-yes, it’s a disease. But it’s also a choice. Every damn day. And that’s the weird part. You don’t have to be ‘ready.’ You just have to be tired enough to try.
And if you’re worried about someone? Don’t wait for them to ‘ask.’ Just say, ‘I’m here. No pressure. But I miss you.’
And if you’re reading this and you’re still drinking? I’m not judging you. I’m just saying: you’re allowed to want more.
And you deserve it.
💛
I’m a nurse. I’ve seen people detox. I’ve held hands during seizures. I’ve watched someone cry because they realized they hadn’t hugged their kid in two years.
It’s not about being ‘weak.’ It’s about being human.
You don’t have to be perfect. You just have to show up.
And if you’re scared? That’s okay. So was I.
One day at a time.
That’s all it takes.
OMG LIZ I CRIED. 😭 I’ve been reading this whole thread and I’m so tired of people acting like recovery is a moral test. You’re not a bad person for needing help. You’re a human who’s been through hell. And you’re still here. That’s not weakness. That’s courage.
Also-I just called my doctor. I’m getting screened tomorrow. I’m scared. But I’m doing it.
Thank you.
@Caitlin Foster-You’re not alone. I called my doctor last week too. Got on naltrexone. First time in 10 years I slept through the night.
One day at a time. 💪