Blood Thinner Dental Procedure Risk Calculator
How to Use This Tool
Select your procedure type and medication details to see if you need to adjust your blood thinner. Based on guidelines from the ADA and major medical organizations.
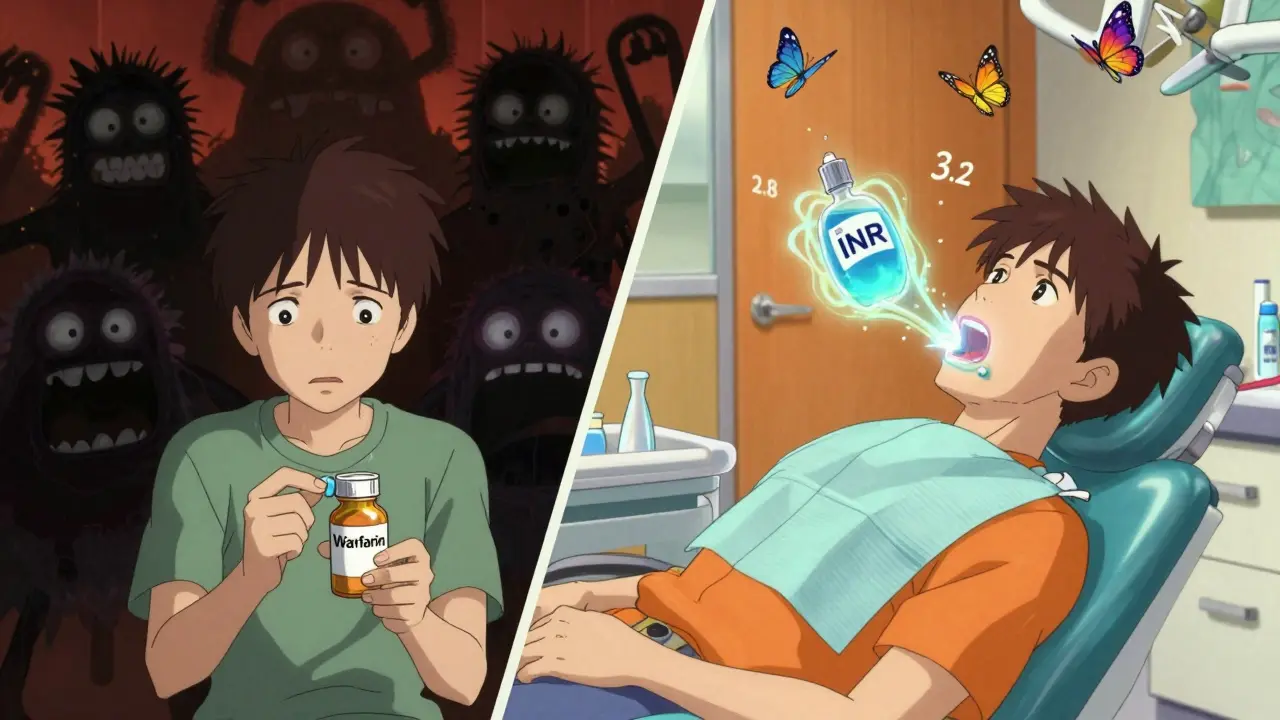
Why You Don’t Need to Stop Your Blood Thinners for Most Dental Work
Many people on blood thinners panic when their dentist mentions a cleaning, filling, or extraction. They assume they need to stop their medication first-sometimes even skipping appointments because they’re afraid of bleeding. But here’s the truth: for the vast majority of dental procedures, stopping your blood thinner is more dangerous than keeping it on.
Back in the 1990s, dentists routinely told patients to pause warfarin or other anticoagulants before any dental work. That practice has changed. Today, major medical and dental organizations-including the American Dental Association (ADA), Stanford Health Care, and the Scottish Dental Clinical Effectiveness Programme (SDCEP)-agree: don’t stop your blood thinner unless you’re having major oral surgery. The risk of a stroke, heart attack, or blood clot from stopping your medication far outweighs the small chance of extra bleeding during a routine procedure.
How Dental Procedures Are Classified by Bleeding Risk
Not all dental work is the same when it comes to bleeding. Procedures are grouped into three clear categories based on how likely they are to cause bleeding:
- Low-risk: Routine checkups, X-rays, teeth cleanings (scaling above the gumline), and making dental impressions. These cause almost no bleeding.
- Low-moderate risk: Fillings, root canals, deep cleanings (scaling and root planing), and placing crowns or bridges. These involve minor gum manipulation but rarely cause serious bleeding.
- Moderate risk: Simple tooth extractions (one to three teeth), gum surgery, or removing a single impacted tooth. These carry a slightly higher chance of bleeding, but still manageable.
Anything beyond that-like multiple extractions, jaw surgery, or complex implant placement-is considered high-risk and may need special planning. But for 9 out of 10 dental visits, you’re in the low or low-moderate risk zone. And for those? No need to change your medication.
What About Your INR Level? (For Warfarin Users)
If you take warfarin (a vitamin K antagonist), your doctor checks your INR-a number that tells how long it takes your blood to clot. The good news? You don’t need to get it perfect. Here’s what’s considered safe:
- Low-risk procedures: INR under 3.5 is fine. Most people on warfarin stay between 2.0 and 3.0 anyway.
- Low-moderate risk: INR under 3.0 is ideal. If you’re at 3.2, it’s still usually okay-just ask your dentist to use extra hemostatic measures.
- Moderate risk: INR under 3.5 is acceptable, especially if your dentist uses gauze, sutures, or a special mouthwash to control bleeding.
If your INR is above 4.0, your dentist should talk to your doctor before proceeding. But even then, stopping warfarin isn’t always the answer. Sometimes, adjusting the dose slightly or delaying the procedure by a few days is safer than stopping cold turkey.
Direct Oral Anticoagulants (DOACs) and Dental Work
More than half of people now on blood thinners take DOACs-drugs like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), or edoxaban (Savaysa). These are easier to manage than warfarin because they don’t require regular blood tests. But they also don’t have a simple number like INR to guide you.
For DOACs, the rule is simple: skip your morning dose on the day of a moderate-risk procedure. For example, if you take apixaban twice a day and have a tooth pulled at 10 a.m., don’t take your 8 a.m. dose. That gives your body time to clear most of the drug. The same applies to single-dose DOACs taken once daily-skip it on the day of the procedure.
For low-risk or low-moderate procedures? Keep taking your DOAC as usual. There’s no benefit to skipping it, and the risk of clotting goes up if you do.
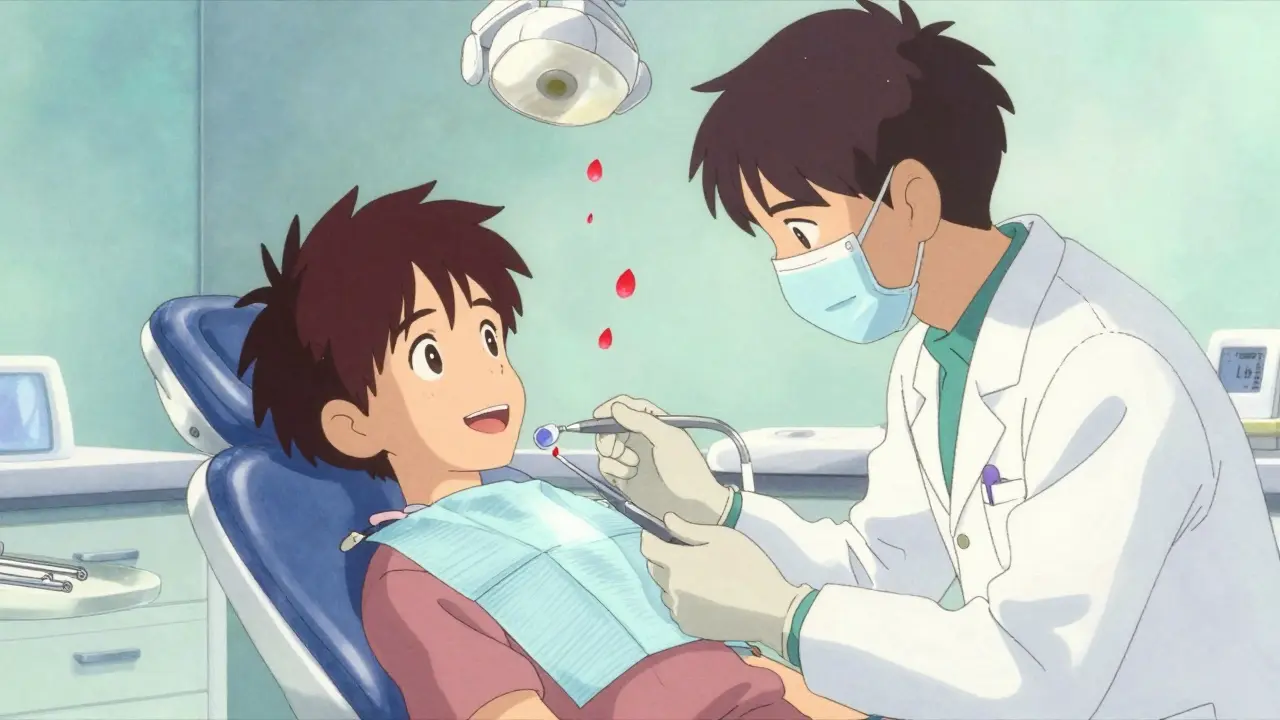
What to Do If You Bleed After the Procedure
Bleeding after a tooth extraction or cleaning is normal-even if you’re not on blood thinners. But if you’re on anticoagulants, you might notice it lasts a bit longer. Here’s how to handle it:
- Place a clean gauze pad over the area and bite down firmly for 30-45 minutes. Don’t keep checking.
- Don’t rinse, spit, or suck through a straw for 24 hours. That can dislodge the clot.
- Use a cold compress on your cheek if swelling happens.
- If bleeding doesn’t slow after 2 hours, use a tranexamic acid mouthwash. This is a special solution (5%) that helps blood clot. Your dentist can make it for you or prescribe it. Swish 10ml for 1-2 minutes, then spit. Repeat every 2 hours if needed.
Most people stop bleeding within a few hours. If it keeps going past 24 hours, call your dentist. But don’t panic-major bleeding is extremely rare.
Drugs to Avoid While on Blood Thinners
Some common medications can make bleeding worse. Be careful with:
- NSAIDs: Ibuprofen (Advil), naproxen (Aleve), and diclofenac. These interfere with platelets and can increase bleeding. Use acetaminophen (Tylenol) instead for pain.
- Aspirin: Even low-dose aspirin can add to the bleeding risk. Don’t start it unless your doctor says so.
- Some antibiotics: Like clarithromycin or fluconazole. These can affect how your liver breaks down warfarin or DOACs, raising your bleeding risk.
- Herbal supplements: Ginkgo biloba, garlic, fish oil, and ginger can thin your blood too. Tell your dentist about anything you take-even “natural” stuff.
Always check with your dentist or pharmacist before starting any new medication, even over-the-counter ones.
Why You Should Never Stop Blood Thinners Without a Doctor’s Advice
Stopping your blood thinner-even for a few days-can be deadly. Studies show that people who stop warfarin or DOACs before minor dental work have a higher chance of having a stroke or blood clot than they do of bleeding badly from a tooth extraction.
One study from UCSD found that holding anticoagulants for a simple extraction didn’t reduce bleeding but did increase the risk of a clot by 3-5%. Another study showed that people who stopped their medication for dental work had a 1 in 100 chance of having a serious clot within 30 days. That’s far worse than the 1 in 1,000 chance of uncontrolled bleeding from a tooth extraction.
Doctors and dentists now agree: the risk of clotting is much higher than the risk of bleeding for most dental procedures. Your heart or brain doesn’t care about your tooth-it cares about blood flow. Don’t risk a stroke just to make a filling easier.
What Your Dentist Should Do (And What You Should Ask)
A good dentist won’t guess. They’ll ask you:
- What blood thinner are you taking?
- What’s your dose?
- When was your last INR test (if on warfarin)?
- Are you taking any other medications or supplements?
- Do you have kidney or liver problems?
Don’t be shy. Bring a list of your medications. If your dentist doesn’t ask these questions, speak up. You have the right to safe care.
Ask your dentist: “Based on what I’m taking and what you’re doing, do I need to change anything?” If they say yes, ask: “Should I talk to my doctor first?” Most of the time, the answer will be: “No change needed.” And that’s exactly what you want to hear.
Real People, Real Cases
It’s not just older adults on blood thinners anymore. More and more younger people are taking them too:
- A 25-year-old athlete with a blood clot after a long flight.
- A 32-year-old woman with atrial fibrillation diagnosed after her first panic attack.
- A 28-year-old new mom who had a pulmonary embolism after delivery.
These patients aren’t “high-risk” just because they’re young. They’re on anticoagulants for a reason-and they need dental care just like anyone else. The guidelines apply to everyone, no matter their age or why they’re on the medication.
Final Takeaway: Keep Taking Your Medication, Stay Informed
You don’t need to fear dental visits because you’re on blood thinners. The evidence is clear: most dental procedures are safe to do while you’re on anticoagulants. Stopping your medication rarely helps and often hurts.
Here’s what you should do:
- Keep taking your blood thinner as prescribed.
- Tell your dentist exactly what you’re on-name, dose, frequency.
- Ask if your procedure is low-risk. If it is, no changes needed.
- For extractions or deep cleanings, ask about tranexamic acid mouthwash.
- Avoid NSAIDs, aspirin, and herbal supplements unless approved.
- If bleeding lasts more than 24 hours, call your dentist.
Modern dentistry has caught up with modern medicine. You don’t have to choose between your heart and your teeth. With the right information, you can have both.







OMG I literally thought I had to stop my Eliquis before every cleaning 😅 I’ve been skipping dentist visits for years bc I was terrified. This post just saved my teeth AND my brain. Thank you so much for writing this!!
Let’s be real - the ADA’s stance on anticoagulant management in dental procedures is a textbook example of evidence-based practice triumphing over antiquated fear-based protocols. The risk-benefit calculus for DOACs versus warfarin in low-to-moderate risk interventions is statistically unambiguous. The notion that INR thresholds above 3.0 necessitate cessation is a relic of the pre-2010 era. Period.
okay so i read this whole thing and like… i think the author is right but also kinda missing the point? like i get that clots are bad but like… my dentist just told me to stop my pill for 3 days before the extraction and now i’m like… wait did i get scammed? also i took ibuprofen after because my face hurt and now i’m scared i’m gonna bleed out in my sleep. help??
Wow. Another feel-good article written by someone who’s never had to clean up a bloody mouth at 2 a.m. while a patient panics. You think bleeding is ‘manageable’? Try being the dentist who has to call 911 because someone’s gushing from three extraction sites and the ER won’t take them without a hematology consult. This isn’t ‘safe’ - it’s reckless under the guise of convenience. And don’t even get me started on people self-medicating with fish oil and ginkgo while ignoring their INR like it’s a Spotify playlist.
As someone from India where dental care is still a luxury for many, this is such a needed message. We have so many people who avoid dentists because they think blood thinners = danger. I’ve told my uncle to keep his rivaroxaban before his cleaning - he was crying he was so scared. Now he’s going next week. Thank you for breaking this down so clearly. We need more of this in our communities.
Oh, so now we’re all supposed to be medical experts because a blog post told us not to panic? How charming. I’m sure the guy who skipped his DOAC before a molar extraction and ended up with a hematoma the size of a grapefruit would agree with your ‘no change needed’ mantra. Bravo. Another hero of misinformation in the age of Google Medicine.
Just wanted to say - this is one of the clearest, most helpful posts I’ve read on this topic. I’m on apixaban and had no idea about skipping the morning dose before extractions. Also, tranexamic acid mouthwash? That’s a game-changer. My dentist didn’t even mention it. I’m printing this out and bringing it to my next appointment. 🙏❤️
This is good info. I’m from Nigeria and we don’t have much of this here. People think if you on blood thinner, you can’t do anything. Even simple cleaning. I will share this with my cousin who is on warfarin. She was scared to go to dentist. Now she will go. Thank you.