Shoulder pain is one of the most common reasons people visit a doctor or physical therapist. And more often than not, it’s not just one problem - it’s a mix of rotator cuff irritation and bursitis working together. You might not know the difference between them, but you definitely feel the pain - especially when you reach for a high shelf, lift your arm to brush your hair, or try to sleep on that side. The good news? Most cases don’t need surgery. With the right approach, you can get back to normal in a few months - no scalpel required.
What’s Actually Going On in Your Shoulder?
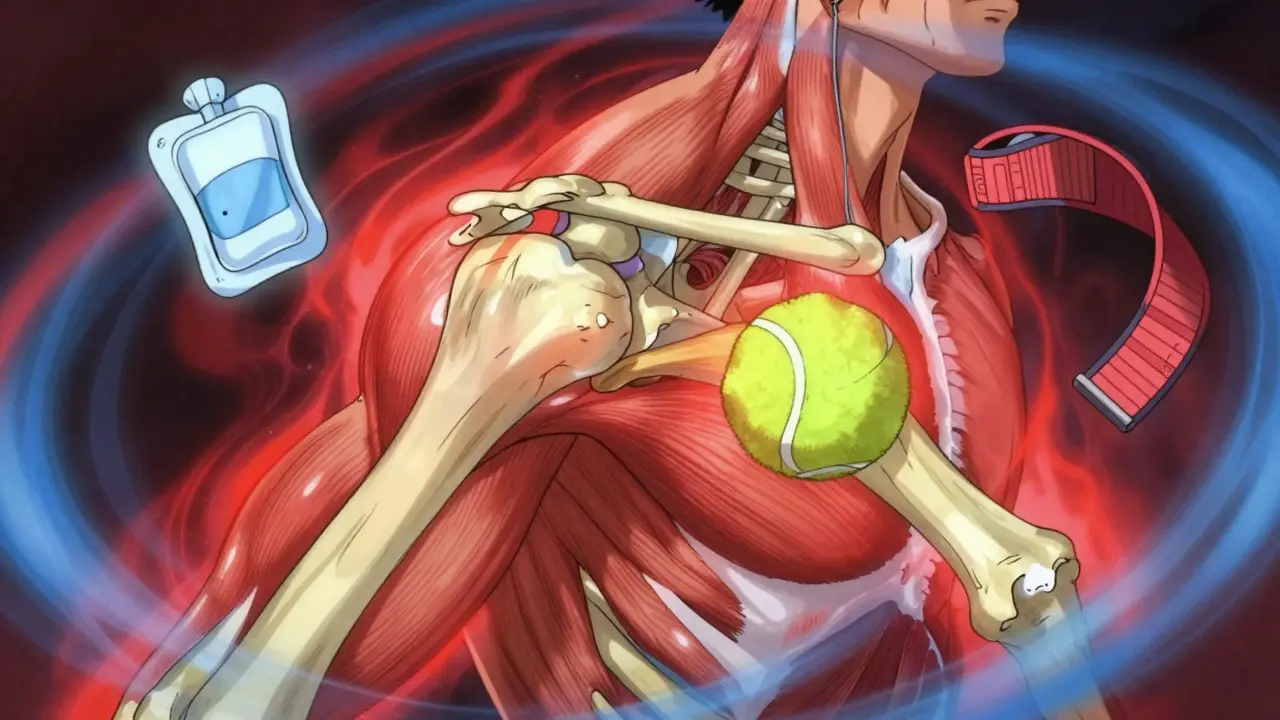
Your shoulder is a ball-and-socket joint, but unlike your hip, it’s not held tightly together by deep bones. Instead, it’s stabilized by four small muscles called the rotator cuff: supraspinatus, infraspinatus, teres minor, and subscapularis. These muscles keep the ball of your upper arm bone (humerus) centered in the socket while you move your arm overhead, behind your back, or out to the side. When these muscles or their tendons get irritated, it’s called rotator cuff tendinitis. Over time, this can lead to tiny tears - especially if you’re over 40. Right above those tendons sits a fluid-filled sac called the subacromial bursa. Its job? To reduce friction as the tendons glide under the bony arch of your shoulder (the acromion). When the bursa gets inflamed - usually from repeated rubbing or sudden trauma - it swells up. Instead of being 1-2 cm thick, it can puff out to 3-4 cm. That’s like putting a tennis ball between your tendons and the bone. Now every time you lift your arm, it’s like grinding sandpaper. This is bursitis. And guess what? It almost always happens alongside rotator cuff irritation. They’re partners in pain.The Pain You Feel - And When It Gets Worse
The classic sign? The painful arc. That’s when you raise your arm out to the side, and between 60° and 120°, it hurts like crazy. Below that, it’s fine. Above it, it eases up again. That’s because this is the exact range where the inflamed bursa and tendons get pinched under the acromion. The pain isn’t sharp - it’s a dull, deep ache that lingers. And yes, it gets worse at night. About 78% of people with this issue report sleep disruption. Lying on the affected shoulder? Forget it. Rolling over? Painful. Sleeping propped up on pillows? That’s your new normal for a while. You might also notice weakness when lifting things, or a clicking sound when you move your arm. But weakness alone doesn’t mean you have a full tear. Many people think if they can’t lift a milk jug, they need surgery. Not true. Most weakness comes from pain inhibition - your brain shuts off the muscle because it hurts. Once the pain drops, strength often comes back on its own.What Doctors Do First - No Surgery Needed
If you go to your GP or an orthopedic specialist, they’ll likely start with the same three-step plan: rest, ice, and anti-inflammatories. No imaging needed yet. You don’t need an MRI just because your shoulder aches. In fact, studies show that up to 40% of people over 60 have rotator cuff tears on MRI - even if they have zero pain. So diagnosis starts with symptoms, not scans.- Rest: Avoid overhead lifting, reaching behind your back, or carrying heavy bags on that side. Not complete rest - you still need to move gently. But stop the things that make it worse.
- Ice: Apply ice for 15-20 minutes, 3-4 times a day. A bag of frozen peas wrapped in a towel works fine. Don’t put ice directly on skin.
- NSAIDs: Ibuprofen (400-600 mg) three times a day for up to 10-14 days. This isn’t a long-term fix, but it helps break the pain-inflammation cycle so rehab can begin.
The Real Key to Recovery: Physical Therapy
Physical therapy isn’t just about doing exercises. It’s about learning how to move differently. The goal isn’t to make your shoulder stronger overnight - it’s to fix the pattern that got you here.- Pendulum exercises: Start within 48 hours. Lean over, let your arm hang loose, and gently swing it in small circles. Do this 5-10 minutes, 3 times a day. It keeps the joint loose without stressing the tendons.
- Scapular retraction: Squeeze your shoulder blades together like you’re trying to hold a pencil between them. Hold for 5 seconds, do 3 sets of 15, twice daily. People who do this consistently heal 30% faster than those who don’t.
- Resistance band work: After 4-6 weeks, start light strengthening with a TheraBand. External rotation (elbow bent at 90°, pulling band away from body) and scaption (raising arm slightly forward at 30°) are the most effective. Use light resistance - 30-50% of your max. Do 2 sets of 15, every other day.
- Range of motion: Use a broomstick or towel to gently guide your arm overhead. Don’t force it. Slow progress beats fast pain.

When Injections Help - And When They Don’t
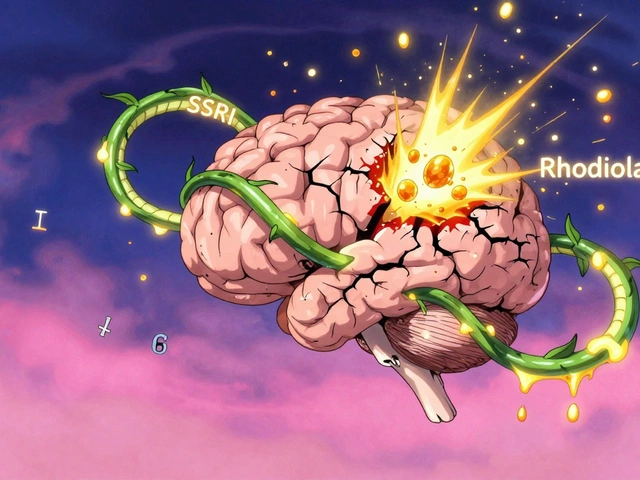
If you’ve done 4-6 weeks of rehab and still can’t sleep or lift your arm, a corticosteroid injection might be next. It’s not a cure - it’s a reset button. The shot, usually a mix of triamcinolone and lidocaine, is guided by ultrasound to make sure it lands right in the bursa. About 65-75% of people get relief for 4-12 weeks. That’s enough time to finally do the rehab without pain. But there are limits. Do more than 2-3 injections a year, and you risk weakening the tendons. There’s an 8% chance of rupture with too many shots. And if you’ve had two injections without lasting improvement, it’s time to rethink the plan - not get a third. Some clinics now offer PRP (platelet-rich plasma) injections after steroid failure. Early data shows it works for about 68% of people, compared to 52% for repeat steroids. But it’s expensive, often not covered by insurance, and still considered experimental by some guidelines.Surgery? Only If You Have to
About 80% of people get better without surgery. That means surgery is the exception, not the rule. You only need it if:- You’ve tried 3-6 months of rehab and injections with no improvement
- You have a full-thickness tear confirmed on MRI - especially if you’re over 60
- You’re a young athlete or manual worker who needs full strength back fast
Who’s Most at Risk?
This isn’t just an “old person” problem. While it’s more common after 40, anyone who does repetitive overhead motion is at risk:- Construction workers - 32% higher risk than average
- Swimmers, tennis players, baseball pitchers - 45% lifetime incidence
- Painters, electricians, warehouse workers
- People who sleep on their side with their arm overhead

What to Avoid
- Don’t ignore pain. Pushing through sharp pain leads to worse damage. - Don’t stop rehab just because you feel better at 6 weeks. Tendons take 3-6 months to fully heal. - Don’t rely on heat alone. Heat feels good, but it doesn’t reduce inflammation. Ice does. - Don’t skip scapular exercises. Weak shoulder blades = bad shoulder mechanics. - Don’t get an MRI too early. You’ll see changes that aren’t causing your pain.Real Success Stories
A 54-year-old carpenter from Bristol had constant pain for 4 months. He couldn’t lift tools. After 14 weeks of physical therapy - with daily scapular exercises and a modified work schedule - he returned to full duty. No surgery. A 37-year-old tennis player had rotator cuff tendinitis after a bad serve. She used daily cryotherapy and eccentric strengthening (slow lowering of the arm with resistance). She was back playing in 10 weeks. Both had one thing in common: they stuck with the plan. Even when it was boring. Even when it hurt a little.Final Takeaway
Shoulder pain from rotator cuff issues and bursitis isn’t a life sentence. It’s a slow, stubborn problem - but one that responds incredibly well to patience and consistency. You don’t need fancy gadgets, expensive treatments, or surgery. You need:- Time - at least 8-12 weeks of consistent rehab
- Correct movement - not just more exercise
- Patience - healing tendons takes months, not days
- Discipline - do the boring stuff, even when you feel okay
Can shoulder bursitis heal on its own without treatment?
Yes, mild cases can improve with rest and avoiding aggravating movements. But without addressing the root cause - like poor shoulder mechanics or muscle weakness - the pain usually comes back. Most people need at least 4-6 weeks of targeted rehab to fully recover and prevent recurrence.
How long does it take to recover from rotator cuff tendinitis?
Recovery typically takes 3-6 months with consistent physical therapy. Some people feel better in 6-8 weeks, but the tendons need longer to rebuild strength and resilience. Rushing back to heavy lifting or sports too soon increases the risk of re-injury by up to 35%.
Is heat or ice better for shoulder bursitis?
Ice is better during the first 2-4 weeks, especially if the shoulder is swollen or hot to the touch. Ice reduces inflammation. Heat can feel soothing but may increase swelling. After the acute phase, gentle heat before exercise can help loosen stiffness, but ice should still follow activity.
Can I still work out with shoulder bursitis?
Yes - but not the way you used to. Avoid overhead presses, bench presses, and any movement that causes pain in the painful arc (60°-120°). Focus on lower body workouts, light cardio, and rehab exercises. Once pain drops below a 3/10, you can slowly reintroduce upper body work with light resistance and perfect form.
Why does shoulder pain get worse at night?
At night, your body is still, and inflammation builds up without movement to circulate fluid. Lying on the affected side also compresses the already swollen bursa and tendons. Plus, without distractions, pain becomes more noticeable. Sleeping on your back with a pillow under the arm or using a body pillow can help reduce pressure.
Do I need an MRI for shoulder pain?
Not usually. Most shoulder pain from bursitis or tendinitis doesn’t show up clearly on MRI - and many people have tears on scans with no pain. An MRI is only needed if you’ve had 3-6 months of rehab with no improvement, or if you have sudden weakness after trauma. Start with a physical exam and rehab first.
Can physical therapy make shoulder pain worse?
It shouldn’t - if done correctly. Mild discomfort during rehab is normal, but sharp, shooting, or worsening pain means you’re pushing too hard or doing the wrong exercise. Always use a 0-10 pain scale: stay below level 5. If pain spikes after exercise, stop and consult your therapist. Poor technique or rushing progression is the most common cause of setbacks.
How often should I do shoulder rehab exercises?
Daily is ideal, especially in the first 4-6 weeks. Scapular exercises and pendulum swings can be done twice daily. Strengthening with bands should be every other day to allow recovery. Consistency matters more than intensity. Doing 10 minutes daily is far better than one 60-minute session per week.