Fosamax vs. Alternatives Comparison Tool
Select a medication and click Compare to see detailed differences between Fosamax and your choice.
Bisphosphonate Class
- Benefit: 30–45% reduction in vertebral fracture risk
- Dosing: Once weekly, 70 mg
- Administration: Oral tablet with full glass of water
Common Side Effects:
- Gastrointestinal irritation
- Rare cases of osteonecrosis of jaw (ONJ)
- Atypical femoral fractures after long-term use
Cost:
$5–$10 per weekDetails will appear here after selection.
When treating osteoporosis, Fosamax (Alendronate) is an oral bisphosphonate that slows bone loss by inhibiting osteoclast activity. But you’re probably wondering if there’s a better fit for your lifestyle, budget, or health profile. This guide walks through how Fosamax stacks up against the most common alternatives, from other bisphosphonates to newer biologics, so you can decide which Fosamax alternatives might work best for you.
What Is Fosamax (Alendronate)?
Fosamax (generic name alendronate sodium) is a prescription medication approved for the prevention and treatment of osteoporosis in post‑menopausal women and men over 50. It belongs to the bisphosphonate class, a group of drugs that bind to bone mineral and make it harder for the body to break down bone tissue.
How Fosamax Works
The drug targets osteoclasts, the cells responsible for bone resorption. By attaching to hydroxyapatite crystals, it interferes with the osteoclasts’ ability to adhere to bone, which reduces the rate of bone breakdown. Over time, this helps maintain or increase bone mineral density (BMD), a key marker of bone strength.
Key Benefits and Risks
- Benefit: Demonstrated 30‑45% reduction in vertebral fracture risk in large clinical trials.
- Convenient dosing: Usually taken once a week with a full glass of water, after an overnight fast.
- Risk: Gastrointestinal irritation, especially if not taken correctly.
- Risk: Rare cases of osteonecrosis of the jaw (ONJ) and atypical femoral fractures after long‑term use.
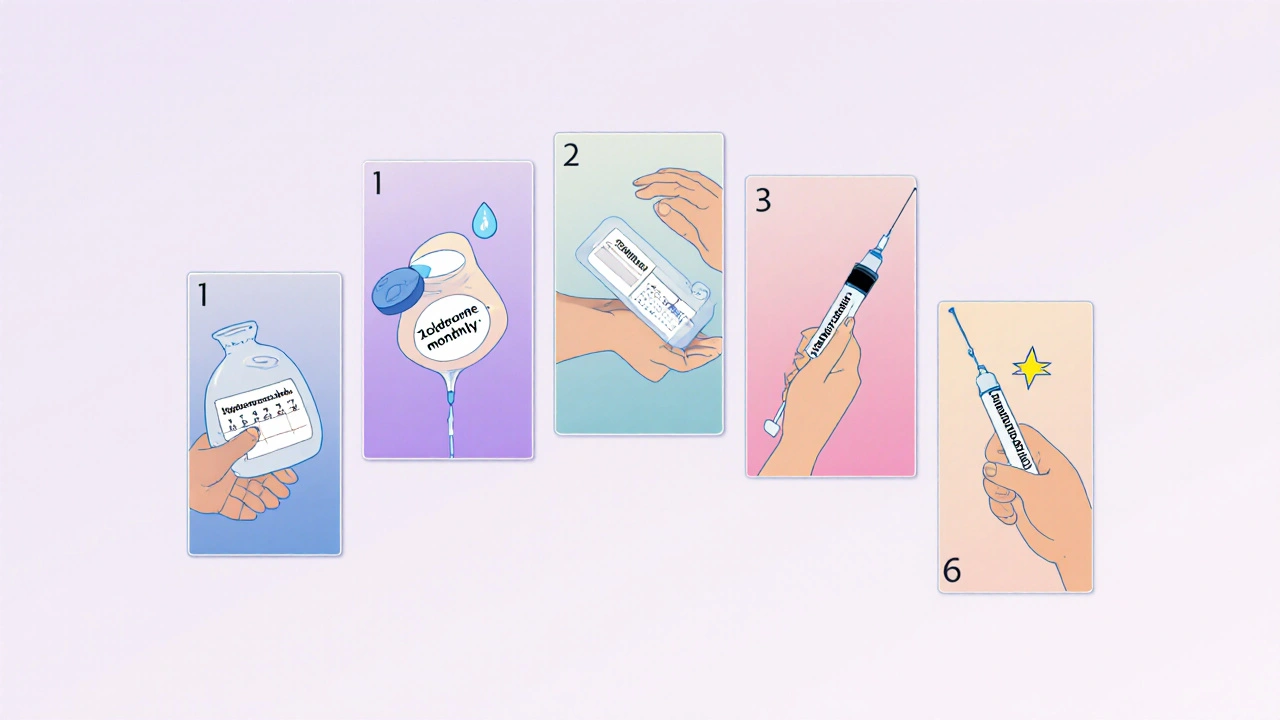
Top Alternatives Overview
Below are the most frequently prescribed options when doctors consider moving patients off Fosamax or starting a different regimen.
Risedronate
Risedronate is another oral bisphosphonate, marketed under brand names such as Actonel. It shares the same mechanism as alendronate but can be taken daily, weekly, or monthly, offering dosing flexibility.
Ibandronate
Ibandronate (Boniva) is an oral bisphosphonate typically prescribed monthly. It is especially useful for patients concerned about gastrointestinal side effects, as the monthly dose is larger but taken less often.
Zoledronic Acid
Zoledronic acid is an intravenous bisphosphonate administered once a year (or once every two years in some protocols). Because it bypasses the gut, it avoids the GI irritation seen with oral agents.
Denosumab
Denosumab (Prolia) is a monoclonal antibody that works differently: it blocks RANKL, a protein that activates osteoclasts. The drug is injected subcutaneously every six months.
Teriparatide
Teriparatide (Forteo) is a recombinant form of parathyroid hormone that actually stimulates new bone formation rather than just slowing loss. It’s given as a daily injection for up to two years.
Side‑Effect Profiles Compared
Understanding adverse events helps you weigh comfort against efficacy. Here’s a quick snapshot:
- Gastro‑intestinal upset: Most common with oral bisphosphonates (Fosamax, Risedronate, Ibandronate). Taking the pill with plenty of water and staying upright for 30 minutes reduces risk.
- Flu‑like symptoms: Frequently reported after the first infusion of Zoledronic acid.
- Skin reactions: Injection‑site erythema can occur with Denosumab and Teriparatide.
- Serious rare events: ONJ and atypical femur fractures are linked to long‑term bisphosphonate use; denosumab may cause rebound bone loss if stopped abruptly.
Choosing the Right Option: Decision Guide
Use the following questions to narrow down the ideal therapy:
- Do you have trouble swallowing pills or a history of stomach ulcer? Consider IV zoledronic acid or a monthly oral option like ibandronate.
- Is adherence a concern? Longer‑interval dosing (monthly, yearly, or six‑monthly) may improve persistence.
- Do you need rapid bone‑building effects, such as after a vertebral fracture? Teriparatide offers anabolic benefits.
- Are you comfortable with injections? Subcutaneous denosumab or daily teriparatide require clinic visits or self‑admin.
- What is your insurance coverage like? Oral generics (alendronate, risedronate) are usually cheaper than biologics.
Discuss these points with your healthcare provider. They’ll also factor in lab results (serum calcium, vitamin D levels) and any comorbidities such as chronic kidney disease, which can limit certain drugs.

Cost & Convenience Snapshot
Here’s a rough US‑centric pricing guide (UK prices are similar after NHS subsidies):
- Fosamax (generic alendronate): $5‑$10 per weekly supply.
- Risedronate (generic): $8‑$12 per weekly supply.
- Ibandronate (generic): $10‑$15 per monthly supply.
- Zoledronic acid: $300‑$400 per yearly infusion (often covered by insurance).
- Denosumab: $1,200‑$1,500 per six‑month injection.
- Teriparatide: $2,500‑$3,500 per month (high‑cost, usually limited to severe cases).
When cost is a major factor, many patients stay on oral bisphosphonates as first‑line therapy. However, if side effects or adherence become problematic, switching to a less frequent or injectable option may save money in the long run by preventing fractures.
Comparison Table
| Drug | Class | Administration | Typical Dose | Main Benefit | Common Side Effects |
|---|---|---|---|---|---|
| Fosamax (Alendronate) | Bisphosphonate | Oral tablet | 70 mg once weekly | Proven fracture risk reduction | GI irritation, rare ONJ |
| Risedronate | Bisphosphonate | Oral tablet | 35 mg once weekly or 150 mg monthly | Flexible dosing schedules | GI upset, esophageal irritation |
| Ibandronate | Bisphosphonate | Oral tablet | 150 mg monthly | Monthly dosing reduces pill fatigue | GI issues, mild musculoskeletal pain |
| Zoledronic Acid | Bisphosphonate (IV) | IV infusion | 5 mg annually | Yearly dosing, bypasses GI tract | Flu‑like symptoms, transient kidney changes |
| Denosumab | RANKL inhibitor | Subcutaneous injection | 60 mg every 6 months | Strong anti‑resorptive effect, works in renal impairment | Injection site reaction, rare hypocalcemia |
| Teriparatide | Anabolic hormone | Daily SC injection | 20 µg daily (max 2 years) | Stimulates new bone formation | Nausea, dizziness, possible osteosarcoma (very rare) |
Frequently Asked Questions
Can I switch from Fosamax to another bisphosphonate without a washout period?
Usually you can transition directly, but doctors often pause for a few days to ensure the stomach is clear of the previous dose. A short “drug holiday” may also be recommended after five years of continuous use.
Is denosumab safer for people with kidney disease?
Yes. Because it’s not cleared by the kidneys, denosumab is often the preferred option when eGFR is below 30mL/min, provided calcium and vitamin D levels are corrected.
What lifestyle changes should accompany medication?
Adequate calcium (1,000‑1,200mg/day) and vitamin D (800‑1,000IU/day) are crucial. Weight‑bearing exercise, smoking cessation, and limiting alcohol also boost bone health.
How long should I stay on any osteoporosis drug?
Most guidelines suggest a drug holiday after 5‑7 years of bisphosphonate therapy if fracture risk has lowered. Newer agents like denosumab or teriparatide have different timelines-typically 2‑4 years for teriparatide, with careful monitoring after stopping.
Are there any head‑to‑head trials comparing Fosamax to denosumab?
The FREEDOM trial for denosumab and the FIT trial for alendronate are separate, but meta‑analyses show denosumab may reduce vertebral fractures slightly more, though at higher cost.








When you’re figuring out bone meds, start with the basics: take the pill with a full glass of water and stay upright for half an hour. It’s the simplest trick that saves you from a lot of tummy trouble.
Whilst the comparison chart is thorough, it neglects to address the paucity of long‑term head‑to‑head trials that truly adjudicate efficacy between bisphosphonates and biologics. A more rigorous evidence base would be advisable.
In the grand tapestry of American medicine, we proudly stride ahead while others still argue about tablets versus injections. The real patriotism lies in demanding the most potent therapy, regardless of cost, because our bones deserve the best.
Honestly, the whole “choose your poison” narrative feels like a melodramatic soap opera. If you can’t tolerate a weekly pill, just pick the yearly IV and stop the drama; your spine will thank you.
Behold, the saga of calcium and collagen! As we wander through the labyrinth of alendronate, risedronate, and denosumab, we confront the eternal question: shall we bow to the oral tablet or embrace the sterile infusion? The answer, dear reader, hinges upon the fragile balance of convenience and courage. One must weigh the bitter sting of gastrointestinal rebellion against the fleeting flu‑like fever after a zoledronic infusion. Yet, beyond the pharmacologic parade, there lies the poetic truth that bone, though inert, whispers loudly when it cracks.
Just pick what works 👍
When counseling patients, I usually highlight adherence data: weekly alendronate has a 60 % persistence rate, whereas monthly ibandronate climbs to 78 %. The side‑effect profile follows the same pattern – less frequent dosing often means fewer GI complaints.
Bottom line: if you’re scared of pills, go IV. If you’re scared of needles, stick with a weekly tablet and set a reminder on your phone.
Here’s the practical rundown: alendronate is cheap and works if you remember the fasting rule; risedronate gives you flexibility – you can take it weekly or monthly; ibandronate cuts down to once a month, which many find easier; zoledronic acid spares you daily pills but requires a clinic visit once a year; denosumab is a semi‑annual shot, great if you have kidney issues; teriparatide is the only anabolic option, but it’s pricey and limited to two years. Choose the schedule that fits your lifestyle, and don’t forget calcium + vit D! 😊
Observing the data, the fracture‑reduction percentages are remarkably similar across oral bisphosphonates, suggesting that the choice often hinges on tolerability and dosing convenience rather than raw efficacy.
One might posit, with a modicum of scholarly gravitas, that the ostensible dichotomy presented herein between “oral tablets” and “injectable marvels” is but a superficial veneer, concealing a deeper, perhaps conspiratorial, stratagem by pharmaceutical conglomerates to fragment the market and engender consumer confusion.
When supporting patients, I stress the importance of a holistic plan – adequate calcium, vitamin D, weight‑bearing exercise, and smoking cessation – in conjunction with whichever medication aligns with their preferences and insurance coverage.
Let’s unpack the whole landscape step by step. First, the pharmacodynamics: alendronate, risedronate, and ibandronate all bind to hydroxyapatite, inhibiting osteoclasts, whereas denosumab hijacks the RANKL pathway, and teriparatide actually stimulates osteoblasts. Second, the dosing frequencies create a compliance gradient – weekly or monthly pills versus a yearly infusion or a semi‑annual injection. Third, side‑effect profiles: oral agents risk esophageal irritation, while IV bisphosphonates can trigger flu‑like symptoms and renal considerations, and denosumab carries a rare hypocalcemia risk. Fourth, cost stratification is stark, ranging from a few dollars a week for generic alendronate to over a thousand dollars for a six‑month denosumab dose. Fifth, patient comorbidities matter – renal impairment nudges you toward denosumab, while a history of gastrointestinal ulceration might push you to the IV route. Sixth, the duration of therapy: many guidelines suggest a drug holiday after five to seven years of oral bisphosphonates, yet denosumab requires a careful taper to avoid rebound bone loss. Seventh, real‑world adherence data shows that less frequent dosing improves persistence; a study showed 80 % adherence for yearly zoledronic acid versus 55 % for weekly alendronate. Eighth, the bone density response: teriparatide uniquely increases trabecular thickness, making it ideal for severe osteoporosis, but its two‑year limit and cost keep it as a second‑line choice. Ninth, the safety monitoring: calcium and vitamin D levels must be optimized for denosumab, while renal function should be checked before zoledronic acid. Tenth, the patient’s lifestyle and preferences often dictate the final selection; a busy professional may prefer a six‑monthly injection over daily pill burden. Eleventh, the insurance landscape can tip the scales, as many plans favor generic bisphosphonates. Twelfth, the clinical evidence: meta‑analyses suggest denosumab may slightly outperform alendronate in vertebral fracture reduction, but the absolute difference is modest. Thirteenth, the emerging data on drug holidays indicates that fracture risk does not surge immediately after stopping bisphosphonates, offering a safety net for long‑term users. Fourteenth, the future horizon includes newer sclerostin inhibitors, which may reshape the treatment algorithm. Finally, the bottom line is that no single agent reigns supreme; therapy must be individualized based on efficacy, safety, cost, and patient preference.
In addressing such a multifaceted therapeutic arena, it is imperative to maintain an inclusive discourse that respects each patient’s autonomy while providing clear, evidence‑based guidance; therefore, clinicians should present all viable options, delineate benefits and risks transparently, and support shared decision‑making.
Regarding the previous extensive exposition, a few grammatical clarifications are warranted: the phrase “the whole landscape step by step” should be hyphenated as “step‑by‑step” for correctness; additionally, “a weekly alendronate” is more idiomatic than “weekly alendronate” when used as a noun phrase; finally, ensure parallel structure in the list of points – each should begin with a consistent verb form (e.g., “First, the pharmacodynamics…”, “Second, the dosing frequencies…”, etc.). These adjustments will enhance readability and precision.
Honestly, the whole medical establishment is part of a grand scheme to keep us dependent on endless injections; they want us to believe only the newest, most expensive drug works while the simple weekly pill is a covert tool of complacency.