Iron Deficiency Anemia is a blood disorder caused by insufficient iron, leading to low hemoglobin levels and reduced oxygen delivery. When the body lacks iron, every organ feels the pinch, including the thyroid gland. This article unpacks the two-way link between iron deficiency anemia and thyroid disorders, highlights overlapping symptoms, and offers a clear roadmap for testing and treatment.
What Exactly Is Iron Deficiency Anemia?
Iron is the core component of Hemoglobin, the protein in red blood cells that carries oxygen. A typical adult woman needs about 12-15g/dL of hemoglobin; dropping below 12g/dL usually signals anemia. The most common cause is a dietary shortfall, chronic blood loss, or impaired absorption.
- Prevalence: Roughly 5‑10% of adults in the UK and up to 25% in women of child‑bearing age.
- Key lab values: Serum ferritin <30µg/L, transferrin saturation <20%.
- Symptoms: Fatigue, pale skin, shortness of breath, restless legs.
Understanding Thyroid Disorders
The thyroid is a butterfly‑shaped gland in the neck that produces Thyroid Hormone, primarily thyroxine (T4) and triiodothyronine (T3). These hormones regulate metabolism, heart rate, and temperature. Any disruption-whether too little (hypothyroidism) or too much (hyperthyroidism)-is labeled a thyroid disorder.
Two forms dominate clinical practice:
- Hypothyroidism is a condition where the thyroid produces insufficient hormone, often reflected by elevated TSH (thyroid‑stimulating hormone) levels.
- Hashimoto's Thyroiditis is an autoimmune attack on the thyroid, the leading cause of hypothyroidism in developed countries.
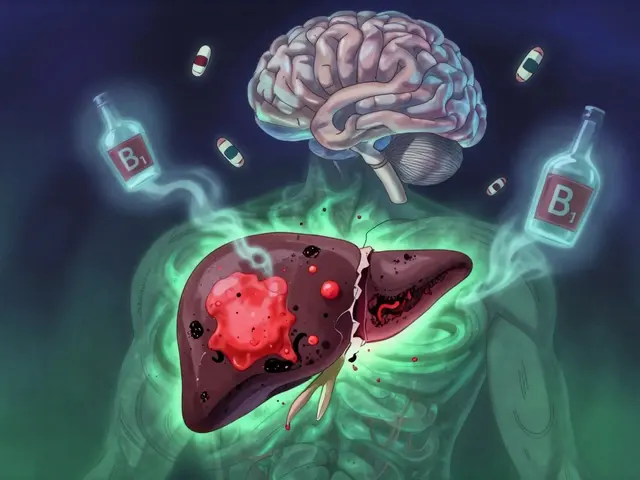
Why Iron Deficiency Impacts Thyroid Function
Iron is a co‑factor for TPO (thyroid peroxidase), the enzyme that adds iodine to tyrosine residues, creating T3 and T4. Low iron reduces TPO activity, hampering hormone synthesis.
Research from UK endocrine societies (2023) shows that patients with ferritin below 30µg/L have a 1.8‑fold higher risk of elevated TSH, even after adjusting for age, gender, and BMI. In practical terms, an iron‑poor diet can push a borderline thyroid into overt hypothyroidism.
Symptoms That Overlap - A Diagnostic Blind Spot
Both conditions share a laundry list of complaints, making it easy to misdiagnose.
| Symptom | Iron Deficiency Anemia | Hypothyroidism |
|---|---|---|
| Fatigue | ✓ | ✓ |
| Cold intolerance | ✗ | ✓ |
| Hair loss | ✓ (severe) | ✓ |
| Pale skin | ✓ | ✗ |
| Weight gain | ✗ | ✓ |
Because fatigue is the most common presenting complaint, clinicians often order a simple CBC and miss the subtle thyroid signs. A thorough history that asks about cold sensitivity, constipation, or slow heart rate can flag the need for thyroid testing.

Lab Work: Connecting the Dots
The ideal work‑up includes both hematology and endocrine panels:
- Complete Blood Count (CBC) - looks at hemoglobin, hematocrit, and red cell indices.
- Serum Ferritin - the gold‑standard iron store marker; values <30µg/L indicate deficiency.
- TSH - primary screen for thyroid function; >4.0mIU/L usually suggests hypothyroidism.
- Free T4 - confirms whether the thyroid is actually under‑producing hormone.
- If TSH is high and free T4 is low, the diagnosis is overt hypothyroidism.
- If TSH is mildly elevated but free T4 is normal, the picture may reflect early disease or iron‑related TPO impairment.
When ferritin is low, treating the iron deficiency first often normalises TSH without needing thyroid medication. This sequential approach avoids lifelong levothyroxine in patients whose hypothyroidism was iron‑driven.
Management Strategies
Effective care hinges on correcting both sides of the equation.
1. Iron Repletion
Oral ferrous sulfate (100mg elemental iron) taken on an empty stomach is the first line. If gastrointestinal upset occurs, switching to ferrous gluconate or a slow‑release formulation helps. Nutrition‑wise, include:
- Red meat, poultry, and fish - highest bioavailable iron.
- Legumes and fortified cereals - good plant sources.
- VitaminC‑rich foods (citrus, bell peppers) - boost absorption.
Avoid coffee or calcium supplements within two hours of iron tablets, as they inhibit uptake.
2. Thyroid Hormone Replacement (if needed)
When TSH remains >4.5mIU/L after 3‑months of iron therapy, start Levothyroxine, a synthetic form of T4, at 25‑50µg daily. Dose adjustments are guided by repeat TSH after 6‑8 weeks.
3. Monitoring and Follow‑up
Repeat CBC, ferritin, and TSH every 8‑12 weeks until both parameters stabilise. Document symptom changes using a simple checklist (energy, temperature sensitivity, mood).
Related Health Topics
Understanding this link opens doors to other interconnected conditions:
- Autoimmune Thyroiditis (Hashimoto's) often co‑exists with celiac disease, which can impair iron absorption.
- Chronic Inflammation raises hepcidin, a hormone that blocks iron release, further aggravating anemia.
- Pregnancy dramatically increases iron demand and can unmask subclinical thyroid disease.
Readers interested in hormone‑nutrient interplay may also explore "Vitamin D and Autoimmune Thyroid Disease" or "Magnesium’s Role in Thyroid Health" as next steps.
Practical Tips for Patients and Clinicians
For patients:
- Keep a symptom diary - note energy levels, temperature changes, and menstrual flow.
- Ask for a combined iron‑thyroid panel if you have chronic fatigue.
- Don’t skip breakfast; a small glass of orange juice with iron improves absorption.
For clinicians:
- Consider ordering ferritin whenever TSH is >4mIU/L, even if CBC looks normal.
- Remember that low ferritin can mask true hypothyroidism; treat iron first in borderline cases.
- Educate patients about timing of supplements and medication to maximise efficacy.

Frequently Asked Questions
Can iron deficiency cause hypothyroidism?
Yes. Iron is essential for thyroid peroxidase, the enzyme that creates thyroid hormones. Low iron reduces TPO activity, which can raise TSH and lead to hypothyroidism, especially in people with borderline thyroid function.
Why do the symptoms of anemia and hypothyroidism overlap?
Both conditions lower the body’s metabolic efficiency. Anemia limits oxygen delivery, while hypothyroidism slows cellular processes. The result is shared complaints like fatigue, hair loss, and poor concentration.
Should I take iron supplements before checking my thyroid?
If you already have a confirmed low ferritin, it’s wise to start iron therapy and repeat the thyroid panel after 8‑12 weeks. This approach can reveal whether the thyroid abnormality resolves with iron alone.
How long does it take for iron therapy to improve thyroid function?
Most patients see a drop in TSH within 2‑3 months if iron deficiency was the primary driver. Full symptom resolution may take 4‑6 months, depending on baseline severity.
Can I take levothyroxine and iron at the same time?
Yes, but separate dosing by at least four hours. Iron can bind levothyroxine in the gut, reducing its absorption, so timing matters.
Are there dietary patterns that help both conditions?
A Mediterranean‑style diet rich in lean meats, fish, leafy greens, nuts, and citrus fruit provides ample iron, iodine, and selenium-nutrients that support healthy thyroid hormone production.






Reading through the connection between iron deficiency anemia and thyroid health really opened my eyes to how intertwined our physiology is and how a simple nutrient shortfall can cascade into a whole series of metabolic challenges you see the hemoglobin drop you feel the fatigue you notice the hair thinning you might even start to think it’s just stress but in reality the thyroid peroxidase activity is starving for the iron it needs to synthesize hormones and when that enzyme falters TSH climbs and the whole feedback loop gets thrown off you end up with that classic hypothyroid picture overlapping with anemia symptoms making diagnosis a real puzzle especially for women who already juggle menstrual losses and dietary gaps the lab work must be thorough you can’t rely on a normal CBC if ferritin is low you’ll see subtle signs and the patient may already be on levothyroxine only to find it’s not working as expected because iron is binding it in the gut therefore timing of supplementation becomes crucial you give iron first wait four to six hours before the thyroid medication and you’ll often see TSH drop within weeks not months the overall treatment plan should be holistic focusing on diet Mediterranean style foods, lean meats, leafy greens, fortified cereals alongside proper iron chelates and monitoring both CBC and thyroid panels regularly to catch improvements early and prevent long‑term complications the take‑away is clear iron isn’t just about red cells it’s a cornerstone for thyroid hormone production and overall metabolic vigor
Honestly this article feels like a patriotic health lecture draped in fancy jargon while ignoring the simple truth that most people in America already have access to iron‑rich foods if you just stop eating junk and start cooking real meals you’ll fix this without the need for endless labs and doctor visits.
Just to add a bit of perspective the relationship between iron and thyroid enzymes is indeed scientifically sound what I’ve seen in my practice is that patients who diligently correct their ferritin levels often experience a smoother normalization of TSH especially when they adhere to proper dosing intervals for levothyroxine and iron so it’s not just about throwing supplements at the problem but about timing and monitoring progress.
It’s fascinating how a deficiency in one mineral can echo through multiple endocrine pathways; think of the body as an orchestra where iron is the conductor for the thyroid section, and if the conductor is absent the music becomes dissonant, leading to fatigue, brain fog, and those classic hypothyroid cues. Addressing iron first not only restores the rhythm but also amplifies the effectiveness of thyroid medication.
Drama alert: ignoring iron is basically self‑sabotage.
Well, if we’re being dramatic, let’s sprinkle some color onto the facts – iron isn’t just a dull mineral, it’s the spark that lights up thyroid fireworks, and without it, the show fizzes out.
While the aforementioned points are generally accurate, it is incumbent upon us, as diligent scholars of physiology, to scrutinize the primary literature and confirm that the causal inference between ferritin levels and thyrotropin elevations holds under rigorous double‑blind conditions, lest we propagate anecdotal conjecture.
Great rundown! I’ve helped a few friends who were stuck in a fatigue loop, and once they started iron supplements and spaced out their thyroid meds, they finally felt their energy bounce back – it’s like resetting the system.
Nice summary 😊
From a philosophical angle, the interplay of iron and thyroid reflects the broader principle that balance in one domain often precipitates harmony elsewhere; neglecting a micronutrient can ripple into macro‑level dysfunction, reminding us to adopt a systems‑thinking approach to health.
In my experience as a collaborative health coach, the key is to personalize the supplementation schedule – I’ve seen patients thrive when they take iron in the morning with vitamin C for absorption, then hold off on levothyroxine until the evening, thus maximizing both therapies without interference.
Let’s get moving on those labs and start fixing those levels – you’ve got this!
I’m curious about the recommended duration for rechecking TSH after iron repletion; is the 8‑12 week window based on clinical trials or expert consensus?
Allow me to point out that the article neglects to mention the role of hepcidin in iron metabolism, which can be upregulated in inflammatory states and thereby impede iron absorption, potentially confounding the perceived efficacy of oral iron supplementation in patients with concurrent autoimmune thyroiditis.
So basically you’re saying iron solves everything? That’s a bit of a stretch, but okay.
Seems like a lot of hype for a mineral.
One must consider the elitist viewpoint that many readers will overlook the subtleties of iron‑thyroid interaction, preferring instead the simplistic notion that a single supplement can replace comprehensive medical evaluation, which is, quite frankly, a dangerous oversimplification.
From an open‑minded perspective, integrating both iron status assessment and thyroid function testing creates a more holistic diagnostic framework, encouraging clinicians to look beyond isolated lab values and appreciate the interconnectedness of endocrine and hematologic health.
Absolutely, leveraging interdisciplinary insights and employing evidence‑based protocols can streamline patient outcomes, especially when we harness terminology like “iron‑thyroid axis” to convey the mechanistic link in a jargon‑rich yet accessible manner.
Thanks for the thorough rundown – I’ll definitely talk to my doctor about checking ferritin before adjusting my thyroid meds.