Rheumatoid arthritis heart risk isn’t just about joint pain - it directly raises the odds of heart attacks, strokes, and early mortality. This article breaks down the biology, shows what the numbers mean, and gives you a clear plan to keep your ticker ticking strong while managing RA.
TL;DR - Quick Takeaways
- People with rheumatoid arthritis face a 1.5‑2× higher risk of cardiovascular disease than the general population.
- Chronic inflammation drives atherosclerosis, endothelial dysfunction, and plaque instability.
- Effective disease‑modifying drugs (DMARDs, biologics) cut heart‑risk by up to 40%.
- Lifestyle tweaks - exercise, heart‑healthy diet, smoking cessation - are essential complements to medication.
- Annual cardiovascular screening (blood pressure, lipid panel, ultrasound) should be part of every RA care plan.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis is a chronic autoimmune disease that primarily attacks synovial joints, causing pain, swelling, and eventual joint damage. The immune system mistakenly unleashes cytokines - inflammatory proteins such as TNF‑α, IL‑6, and IL‑1β - that erode cartilage and bone. While the joints scream, the rest of the body listens, too.
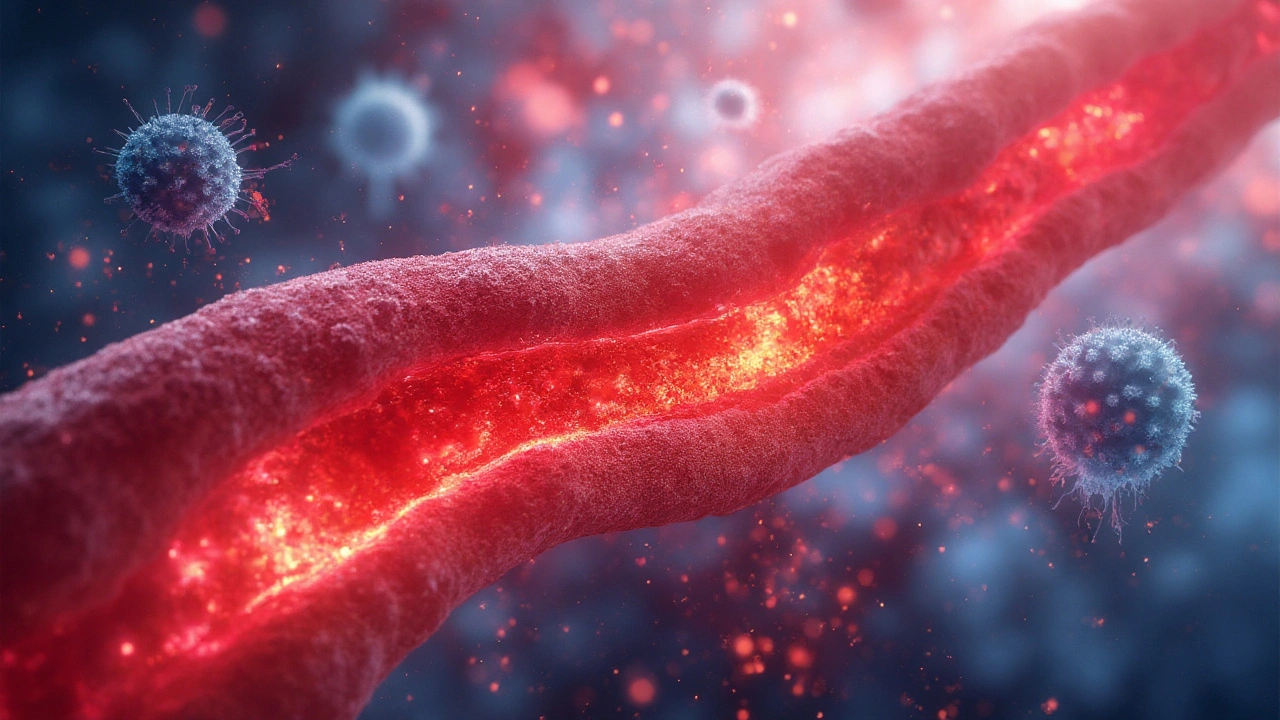
Why the Heart Gets Caught Up
Inflammation is the common thread linking RA to heart disease. In the blood vessels, the same cytokines that devastate joints also trigger endothelial dysfunction, a condition where the inner lining of arteries loses its ability to regulate blood flow and prevent clot formation. This dysfunction accelerates atherosclerosis, the buildup of fatty plaques inside arterial walls.
Three mechanisms dominate:
- Accelerated plaque formation: Inflammatory cells infiltrate arterial walls, depositing cholesterol and creating unstable plaques.
- Pro‑thrombotic state: High levels of fibrinogen and platelet activation raise the chance of clotting, leading to myocardial infarction or stroke.
- Impaired vascular repair: Endothelial progenitor cells are reduced, limiting the vessel’s natural healing capacity.
The Numbers Behind the Risk
Large cohort studies from the UK, Sweden, and the US consistently show that RA patients experience a 1.5‑to‑2‑fold increase in cardiovascular events compared with age‑matched controls. A 2023 meta‑analysis of 45 studies reported:
- Cardiovascular mortality: 1.7× higher
- Coronary artery disease incidence: 38% higher
- Stroke risk: 22% higher
These figures hold even after adjusting for traditional risk factors like hypertension and high LDL cholesterol. In other words, RA adds an independent cardiovascular burden.
Medication Matters: How Treatment Alters Heart Risk
Not all drugs are created equal when it comes to heart health. The two main classes used to tame RA are:
- DMARDs (Disease‑Modifying Antirheumatic Drugs) - conventional agents like methotrexate, sulfasalazine, and leflunomide.
- Biologic therapies - targeted antibodies against TNF‑α, IL‑6, or CD20.
Both classes reduce systemic inflammation, but they differ in speed and depth of control. Recent trials (e.g., the 2022 CIRT‑RA study) show that patients on biologics experience a 30‑40% lower relative risk of major cardiovascular events compared with those on NSAID‑only regimens.
| Treatment | Relative Risk Reduction (RRR) | Primary Mechanism |
|---|---|---|
| Methotrexate (DMARD) | ~20% | Reduces systemic cytokine levels, improves endothelial function |
| TNF‑α Inhibitor (Biologic) | ~35% | Blocks key inflammatory pathway, stabilises plaques |
| IL‑6 Receptor Antagonist | ~30% | Lowers CRP and fibrinogen, reduces pro‑thrombotic state |
| Long‑term NSAIDs | ↑10% (risk increase) | Elevates blood pressure, worsens renal function |
Lifestyle Levers: What You Can Do Today
Medication is only half the battle. The following habits have the strongest evidence for offsetting RA‑related heart risk:
- Exercise regularly: 150 minutes of moderate aerobic activity per week reduces CRP by ~25%.
- Adopt a Mediterranean diet: High in omega‑3 fatty acids, nuts, and olive oil; linked to a 15% drop in cardiovascular events among RA patients.
- Quit smoking: Smoking not only worsens joint damage but also triples heart‑disease risk in RA.
- Maintain healthy weight: Each BMI point above 25 adds ~8% extra cardiovascular risk.
- Control blood pressure and lipids: Tight targets (BP <130/80 mmHg, LDL <70 mg/dL) are recommended for high‑risk RA groups.
Screening & Monitoring: Keeping an Eye on the Heart
Because RA patients develop heart disease silently, proactive screening is vital. Ideal annual checks include:
- Blood pressure measurement
- Lipid panel (total cholesterol, LDL, HDL, triglycerides)
- High‑sensitivity C‑reactive protein (hs‑CRP) as an inflammation marker
- Carotid ultrasound to detect early plaque buildup
- Electrocardiogram (ECG) for arrhythmia detection
When any of these markers rise, rheumatologists should coordinate with cardiologists to adjust therapy promptly.
Emerging Research: What’s on the Horizon?
Scientists are digging deeper into the RA‑heart link. Two promising avenues:
- JAK inhibitors: Early data suggest they may lower atrial fibrillation risk while controlling joint disease.
- Microbiome modulation: Gut bacteria influence systemic inflammation; probiotic trials aim to reduce both RA flares and atherosclerotic progression.
While still experimental, these fields highlight that the next decade could bring even more heart‑protective options for RA patients.
Putting It All Together: A Practical Checklist
Use this simplified action plan each year:
- Visit rheumatologist - confirm disease activity is low (DAS28 <3.2).
- Review medication - aim for a DMARD or biologic that controls inflammation.
- Get a cardiovascular screen - BP, lipids, hs‑CRP, carotid ultrasound.
- Adopt heart‑healthy habits - diet, exercise, quit smoking.
- Schedule follow‑up with cardiologist if any risk marker rises.
Following these steps dramatically cuts the odds of a heart attack or stroke, turning a potentially fatal double‑whammy into a manageable health duo.
Frequently Asked Questions
Why does rheumatoid arthritis increase heart disease risk?
RA fuels chronic systemic inflammation, which damages blood‑vessel walls, speeds up atherosclerosis, and makes blood more prone to clotting. Those processes raise the chance of heart attacks and strokes independently of traditional risk factors.
Can RA medications lower my heart risk?
Yes. DMARDs such as methotrexate and biologic agents that block TNF‑α or IL‑6 have been shown to cut cardiovascular events by 20‑40% compared with untreated or NSAID‑only regimens. The key is achieving tight control of inflammation.
Should I get a heart scan even if I feel fine?
Absolutely. Early plaque often shows up on carotid ultrasound or coronary calcium scoring before symptoms appear. Annual screening helps catch problems early and guides treatment adjustments.
Do lifestyle changes matter if I’m on medication?
Lifestyle is a critical partner to meds. Exercise, a Mediterranean‑style diet, and smoking cessation can lower CRP by up to a quarter and further reduce cardiovascular risk beyond what drugs achieve alone.
What are the warning signs of heart trouble in RA patients?
Chest pain or pressure, shortness of breath, sudden weakness in a limb, and unexplained fatigue can all signal heart issues. Because RA can mask symptoms, any new or worsening sign should trigger immediate medical review.
Is there a future cure that might also protect the heart?
Research into JAK inhibitors and gut‑microbiome therapies is promising, but a definitive cure is still years away. Meanwhile, the best strategy remains tight inflammation control with existing DMARDs/biologics and heart‑healthy living.








Interesting breakdown, but honestly, most docs in the US don’t even check CRP for RA patients unless you beg. I’ve been managing this for 8 years and my rheum only brought up heart risk last year-after I had a borderline lipid panel. Meanwhile, my cousin in Bangalore gets full cardiac workups every 6 months just because he’s on methotrexate. System’s broken.
Also, Mediterranean diet? Try explaining that to your mom who thinks ghee is medicine and roti is the only real food. Good luck.
Let’s cut through the fluff. The real issue isn’t RA-it’s the pharmaceutical-industrial complex’s obsession with biologics while ignoring the fact that 60% of RA patients are on Medicaid or uninsured. You cite ‘30–40% risk reduction’ like it’s gospel, but where’s the data on real-world adherence? Most people can’t afford biologics, can’t get referrals for cardiac ultrasounds, and are told to ‘just exercise’ while working two jobs.
This isn’t medicine. It’s a luxury pamphlet for people who can afford to care.
Oh wow, another ‘RA causes heart disease’ article written by some Ivy League doc who’s never met a real person with this condition. Let me guess-you also think ‘Mediterranean diet’ is the cure-all for people who can’t afford salmon and olive oil? Meanwhile, in this country, half the patients are on canned soup and frozen pizza because that’s all SNAP covers.
And don’t even get me started on NSAIDs. Yeah, they’re ‘bad,’ but try telling someone in rural Ohio who can’t drive to a clinic for a biologic injection that their $5 ibuprofen is killing them. This is class warfare disguised as science.
Hey everyone-I’ve had RA for 12 years and I’m 57 now. I’m alive because I took methotrexate, stopped smoking cold turkey, and started walking 30 mins every day-even when my knees screamed. I didn’t have fancy biologics, but I had consistency.
Also, I got my first cardiac ultrasound at my rheum’s office-free, no referral needed. Don’t let the noise make you think you need perfection. Small steps matter. If you’re reading this and you’re scared? You’re not alone. Just start somewhere. Even a 10-minute walk counts.
And yes, I still eat pizza. But I also eat lentils. Balance, not perfection.
They’re lying to you. The inflammation isn’t from your immune system-it’s from glyphosate in your food, 5G towers, and the CDC’s secret agenda to push biologics so Big Pharma can sell you lifetime subscriptions to $20,000/month drugs.
My neighbor’s cousin’s dog got arthritis and they gave it turmeric and CBD oil-now it’s running like a puppy. Meanwhile, you’re getting MRIs and blood draws like a lab rat.
And don’t get me started on ‘Mediterranean diet.’ That’s just a fancy way of saying ‘eat like a European rich person.’ Most of us can’t afford olive oil that costs more than our rent.
They want you dependent. Break the cycle. Stop trusting doctors. Start trusting your gut. And burn this article.
Just wanted to say thanks to Brian O for saying what I’ve been thinking. I’ve been on methotrexate since 2018. My BP was through the roof, my triglycerides were insane, and my doctor never mentioned heart risk until I asked. Once I started walking after dinner and cut out soda? My CRP dropped 30% in 4 months.
It’s not glamorous. It’s not a biologic. But it’s real. And if you’re reading this and feel overwhelmed? You don’t have to fix everything today. Just one thing. One small thing. That’s enough.