Drug shortages aren’t just inconvenient-they’re dangerous. When a life-saving injectable antibiotic or chemotherapy drug disappears from hospital shelves, patients don’t get treated on time. Some die. In 2022, the FDA recorded 245 drug shortages, with over half involving sterile injectables used in emergency rooms, ICUs, and during surgery. The cost? More than $216 million extra in healthcare spending that year. And it’s not getting better. The system we’ve been using-lean, global, and hyper-focused on cutting costs-isn’t built to handle shocks. It’s time to stop reacting and start building resilience into the drug supply.
Why the current system keeps failing
The modern drug supply chain was designed for efficiency, not safety. Most active pharmaceutical ingredients (APIs)-the core chemical components of medicines-are made in just two countries: China and India. Together, they supply 28% of the APIs used in U.S. drugs. That sounds fine until a flood, a political dispute, or a factory fire shuts down one facility. Then, thousands of doses vanish overnight. And because companies rely on just-in-time delivery, there’s no buffer. No backup. No plan B. Worse, only 12% of pharmaceutical companies can see beyond their immediate suppliers. That means if a raw material supplier in Vietnam gets hit by a cyberattack, the company making your blood pressure pill won’t even know it’s coming until their production line stops. This isn’t speculation. It’s fact. The Healthcare Distribution Alliance found a 214% spike in cyberattacks targeting drug supply chains between 2020 and 2023. One breach can ripple across continents.What resilience actually means
Building resilience isn’t about stockpiling every drug under the sun. That’s expensive and wasteful. It’s about designing a system that can bend without breaking. The National Academies of Sciences laid out three pillars: anticipation, planning, and risk management.- Anticipation means knowing where your risks are before they happen. That requires mapping every step of the supply chain-from the mine that produces a chemical compound to the warehouse that ships the final pill.
- Planning means deciding ahead of time: Which drugs are critical? Who are our backup suppliers? What alternatives exist if one formulation runs out?
- Risk management means putting real strategies in place: dual sourcing, buffer stocks, cybersecurity protocols, and regulatory flexibility.
The most effective systems don’t rely on one fix. They layer multiple strategies together.
Four proven strategies to build resilience
1. Diversify suppliers-not just geographically, but technically
Relying on one supplier for a critical drug is like having one bridge to your city. If it collapses, you’re stuck. The solution? Have at least three suppliers for each essential medicine, spread across different continents. But it’s not enough to just find more factories. You need different technologies too. For example, if your API is made using a complex chemical synthesis process, have a second supplier using a fermentation-based method. That way, if one process fails due to regulatory changes or equipment breakdown, the other can pick up the slack.Merck’s 2022 initiative to bring API production for 12 key antibiotics back to the U.S. didn’t just reduce risk-it created redundancy. They now produce 95% of these drugs domestically. Yes, costs went up by 31%. But when a global shortage hit, they kept delivering. Hospitals didn’t scramble. Patients got their treatment.
2. Build buffer stocks for the most critical drugs
Not all drugs need a six-month stockpile. But for life-saving injectables-like epinephrine, insulin, or antibiotics used in sepsis-having 6 to 12 months of supply on hand is non-negotiable. The cost? Around $3.5 billion annually to stockpile everything. But if you focus only on the top 50 most critical drugs? That drops to under $1 billion. And it prevents 45% of shortages.The HHS 2024 plan is starting to do this right. They’re allocating $520 million to build domestic stockpiles for 50 essential medicines, aiming for 40% domestic API production by 2027. That’s not just insurance-it’s a strategic investment.
3. Use technology to see the whole chain
You can’t fix what you can’t see. That’s why supply chain mapping is the highest-return investment in resilience. Companies with full visibility-from raw materials to final packaging-report 32% fewer disruptions, even though they spend only 8% of their resilience budget on this.AI-powered forecasting tools now predict disruptions with 83% accuracy up to 30 days ahead. Pfizer used this tech across 150 distribution centers and cut stockouts by 38%. The catch? It took $220 million and 18 months to implement. But the payoff? Fewer emergency deliveries, less waste, and more predictable care.
4. Prepare alternatives before you need them
Sometimes, the best solution isn’t more of the same drug-it’s a different one. If your hospital runs out of Drug A, can they switch to Drug B? Is it FDA-approved? Is it in the formulary? Is the pharmacy trained to use it?Only 15% of hospital formularies include pre-approved alternatives for critical drugs. That’s a failure of planning. The solution? Regularly review and update formularies to include at least one alternative for every high-risk medication. Train staff. Update protocols. Test it in drills. When a shortage hits, you don’t want to be figuring out alternatives for the first time.
What doesn’t work
Resilience isn’t about throwing money at the problem. It’s about smart, targeted action.- Just stockpiling everything is too expensive and leads to expired inventory.
- Only reshoring production adds 25-40% to costs and isn’t practical for every drug.
- Waiting for shortages to happen before acting? That’s not resilience-that’s negligence.
And here’s the biggest myth: that this is only a U.S. problem. It’s not. The European Medicines Agency has already forced manufacturers to create parallel supply chains for the EU and U.S. markets. If you’re a global company, you’re already being forced to adapt. The question is: Are you ahead of the curve-or playing catch-up?
The hidden cost of inaction
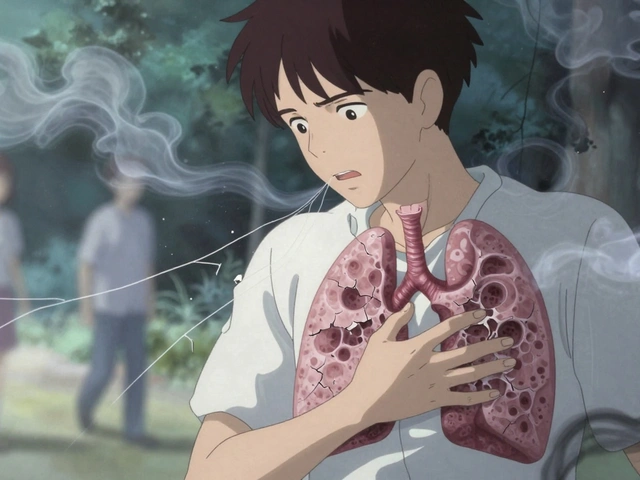
Every shortage has a human price. A cancer patient waits weeks for a chemo drug. A newborn in the NICU gets a substitute antibiotic with higher side effects. An elderly patient on dialysis misses a dose because the saline solution isn’t available. But there’s also a financial cost. The U.S. spends $1.4 trillion a year on prescription drugs. Yet, supply chain resilience gets just 1.2% of industry R&D spending. Meanwhile, shortages cost the system over $200 million annually in extra care, emergency deliveries, and lost productivity.It’s not just about saving money. It’s about saving lives. And it’s not a future problem. It’s happening now.

What’s changing in 2025 and beyond
Regulators are finally stepping in. The FDA’s new draft guidance, due for full implementation by Q3 2025, requires every manufacturer to conduct annual vulnerability assessments. If you can’t show you’ve mapped your supply chain and identified risks, you won’t get approval for new drugs.Then there’s Medicare. In 2024, CMS proposed a rule that would tie reimbursement to supply chain transparency. By 2026, manufacturers will have to disclose their entire supply chain-from raw materials to final packaging-for any drug covered under Medicare. That’s $80 billion in spending now under scrutiny.
And it’s not just regulation. Venture capital is pouring in. $2.3 billion went to supply chain visibility startups in 2023 alone. AI tools are getting smarter. Governments are coordinating. The Pharmaceutical Security Institute now includes 17 countries working on harmonizing standards for 200 critical medicines.
This isn’t a trend. It’s a transformation.
Where do we go from here?
Resilience isn’t a project. It’s a mindset. It’s built into the DNA of how companies make, distribute, and track drugs. It requires:- Leadership that treats supply chain risk as seriously as drug safety.
- Investment in mapping and AI-not just as tools, but as core infrastructure.
- Regulatory alignment across borders so companies aren’t forced to build separate systems.
- Hospitals that demand resilience from their suppliers.
The companies that survive the next crisis won’t be the ones with the cheapest drugs. They’ll be the ones who planned ahead. Who diversified. Who mapped. Who prepared.
The next shortage isn’t a question of if. It’s a question of when. Are we ready?
What causes most drug shortages today?
Most shortages are caused by manufacturing disruptions, especially in facilities that produce active pharmaceutical ingredients (APIs). Over 72% of API manufacturing for U.S. drugs happens overseas, with 28% concentrated in China and India. Single-source suppliers, lack of backup production, cyberattacks, and regulatory delays are the top contributors. Sterile injectables are especially vulnerable because they require highly controlled environments, and even minor contamination can shut down an entire production line.
Is reshoring drug manufacturing the best solution?
Reshoring helps, but it’s not a silver bullet. Bringing API production back to the U.S. increases costs by 25-40%, making it viable only for the most critical drugs-like life-saving injectables or antibiotics. A hybrid approach works better: reshoring a small number of high-risk products while diversifying suppliers internationally. This cuts costs by half compared to full reshoring and prevents 85% of shortages. It’s about smart prioritization, not blanket relocation.
How much buffer stock is needed to prevent shortages?
For the most critical drugs-those used in emergencies, ICUs, or surgeries-a 6- to 12-month supply is recommended. Stockpiling everything would cost over $3.5 billion annually. But focusing only on the top 50 essential medicines reduces that to under $1 billion and prevents 45% of shortages. The key is identifying which drugs truly need buffers, not just hoarding everything.
Can AI really predict drug shortages?
Yes, and it’s already being used. AI models analyzing supplier data, weather patterns, shipping delays, and regulatory filings can predict disruptions up to 30 days in advance with 83% accuracy. Companies like Pfizer have used this to reduce stockouts by 38%. The technology isn’t perfect, but it’s far more reliable than human guesswork-and it’s getting better every year.
Why is cybersecurity important for drug supply chains?
Cyberattacks can shut down entire manufacturing lines. Between 2020 and 2023, attacks on pharmaceutical supply chains increased by 214%. A ransomware attack on a supplier in India once halted production of a common antibiotic for six weeks. The Healthcare Distribution Alliance now requires all partners to follow NIST cybersecurity standards. Ignoring this isn’t just risky-it’s negligent.
What’s the role of government in fixing drug shortages?
Government sets the rules and provides incentives. The FDA now requires annual vulnerability assessments from manufacturers. The HHS is funding $520 million to build domestic production for 50 critical drugs. Medicare may soon tie reimbursement to supply chain transparency. Without regulation, companies won’t invest. But with clear rules and financial support, the industry can change.
Are generic drugs more vulnerable to shortages?
Yes, and that’s counterintuitive. Generic drugs make up 90% of prescriptions but only 20% of spending. Because they’re low-margin, manufacturers cut costs aggressively-using single suppliers, minimal inventory, and overseas facilities. That makes them more fragile. Over 60% of shortages involve generics, especially injectables. The system rewards cheapness over resilience, and that’s the core problem.
What can hospitals do to prepare for shortages?
Hospitals should create a critical drug list and identify pre-approved alternatives for each. Train pharmacists and clinicians on substitution protocols. Build relationships with multiple distributors. Track inventory daily, not weekly. And demand transparency from suppliers. When a shortage hits, the hospital that’s already planned will keep operating. The one that waits won’t.