Post-Operative Dizziness Risk Assessment Tool
Assess Your Dizziness Risk
Results will appear here after assessment
When you wake up after surgery, post-operative dizziness is a common feeling of light‑headedness or unsteadiness that can last from a few minutes to several hours. It’s uncomfortable, but with the right know‑how you can keep it under control and get back on your feet faster.
Key Takeaways
- Identify the top three physiological reasons for dizziness after anesthesia.
- Follow a step‑by‑step protocol for safe sitting, standing, and walking.
- Know which drinks, foods, and simple exercises help stabilise blood pressure.
- Recognise red‑flag symptoms that require immediate medical attention.
- Coordinate with your anesthesiologist and nurse to adjust any medications that may be contributing.
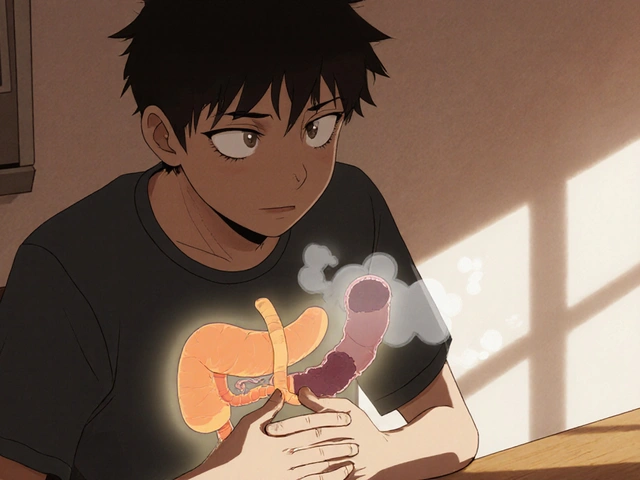
Why Does Dizziness Happen After Anesthesia?
Understanding the "why" makes the "how" a lot easier. Three main mechanisms drive that woozy feeling:
- Blood pressure drops - especially orthostatic hypotension when you move too quickly.
- Dehydration - fluids are often restricted before surgery, and anesthesia can increase urine output.
- Medication side effects - opioids, anti‑nausea drugs, and certain muscle relaxants can all affect the vestibular system.
Each factor interacts with the vestibular system, the inner‑ear network that tells your brain where you are in space. When blood flow or medication interferes with that system, you feel off‑balance.
Step‑by‑Step Recovery Routine
Follow this routine the first 24 hours after surgery. It’s designed to keep blood pressure steady, boost hydration, and protect the inner ear.
1. Prepare Your Environment
- Keep the room temperature moderate; extreme heat or cold can widen blood vessels and worsen instability.
- Have a sturdy chair, a night‑stand with a glass of water, and a phone within arm’s reach.
- Turn on a night‑light so you can see clearly when you get up.
2. The Sit‑Up‑and‑Wait Technique
When the nurse says you’re cleared to sit, do this:
- Lift your legs onto the side of the bed while keeping your back flat.
- Stay seated for at least two minutes. If you feel light‑headed, sit a bit longer before attempting to stand.
- Take a slow, deep breath; the extra oxygen helps stabilise the heart rate.
During this time, check your blood pressure if a monitor is available. Aim for a systolic reading above 100mmHg before moving.
3. Standing Up Safely
When you feel ready:
- Place both feet flat on the floor, shoulder‑width apart.
- Shift weight onto your heels, then slowly rise using the armrests for support.
- Pause for 30seconds before taking a few steps. If dizziness returns, sit down and repeat the sit‑up‑wait cycle.
4. Light Activity and Walking
Short walks (5-10meters) help circulation and signal the brain that it’s safe to increase upright time. Walk at a comfortable pace, holding onto a wall or rail if needed. Gradually lengthen the distance each hour.

Hydration and Nutrition Strategies
Re‑hydrating is a cornerstone of dizziness management. Aim for 1.5-2liters of fluid over the first 24 hours, unless your surgeon tells you otherwise.
- Water with electrolytes - sports drinks or oral rehydration solutions replace sodium lost through urine.
- Warm herbal teas - ginger or peppermint tea can soothe nausea while adding fluid.
- Small, frequent meals - toast, crackers, or a banana provide glucose without overloading the stomach.
Avoid caffeinated or alcoholic beverages in the first day; they can dehydrate you further and exacerbate blood‑pressure swings.
Medication Review: What to Watch For
Many post‑surgery prescriptions can unintentionally trigger dizziness. Keep this quick checklist handy and discuss any concerns with the nurse or anesthesiologist.
| Medication | Why It Can Cause Dizziness | Tip to Minimise |
|---|---|---|
| Opioids (e.g., morphine) | Depresses the central nervous system, lowers blood pressure | Take with food; request the lowest effective dose |
| Anti‑emetics (e.g., ondansetron) | Can affect inner‑ear signaling | Stay hydrated; monitor for any new ringing in ears |
| Muscle relaxants (e.g., cyclobenzaprine) | Cause sedation and reduced proprioception | Limit activity until the drug clears (usually 24hrs) |
| Blood pressure meds (e.g., lisinopril) | May drop systolic pressure too quickly | Check BP before standing; keep a log for the nurse |
If you’re prescribed any of the above, ask the healthcare team whether a dose adjustment or an alternative can reduce the dizzy side‑effects.
When to Call the Doctor
Most light‑headedness resolves within a few hours, but certain signals mean you need professional help right away:
- Chest pain, palpitations, or shortness of breath.
- Sudden, severe headache that doesn’t improve with rest.
- Persistent vomiting that prevents fluid intake.
- Blurred vision or loss of balance that continues after the first 24 hours.
- Feeling faint while sitting or lying down, not just when standing.
Call your surgeon’s office, the on‑call anesthesiologist, or go to the nearest emergency department if any of these occur.

Longer‑Term Strategies for Ongoing Recovery
Even after the initial dizziness fades, a few habits keep you steady for weeks ahead:
- Gradual upright training - Spend 5‑10minutes each day sitting up, then standing, increasing time slowly.
- Gentle vestibular exercises - Head‑turning and eye‑movement drills improve inner‑ear coordination. A simple one: sit, keep eyes fixed on a point, turn your head slowly left‑right for 30seconds.
- Maintain normal fluid intake - Aim for at least 2L per day once cleared for a regular diet.
- Balanced diet rich in potassium - Bananas, oranges, and leafy greens help regulate blood pressure.
- Regular light activity - Short walks, gentle stretching, or stationary cycling keep circulation smooth.
Recap of the Practical Plan
Put everything together in a quick reference you can keep by your bedside:
- Check vital signs (BP, pulse) before each position change.
- Follow the Sit‑Up‑and‑Wait routine: 2‑minute sit, then slow stand.
- Drink 200ml of electrolyte water every hour.
- Take prescribed meds with food, and note any dizzy side‑effects.
- Call for help if you notice chest pain, severe headache, or persistent vomiting.
Stick to this checklist, stay hydrated, and communicate openly with the care team - you’ll be back to normal much sooner.
Frequently Asked Questions
Is it normal to feel dizzy the first night after surgery?
Yes. Up to 40% of patients report light‑headedness in the first 12hours because anesthesia lowers blood pressure and fluids are limited before the operation. The feeling should subside as you start moving and hydrating.
Can I drink coffee to wake up faster?
Coffee can increase heart rate but also acts as a diuretic, which may worsen dehydration. It’s safer to start with water or an electrolyte solution, then add coffee later if you tolerate it well.
What if my dizziness lasts more than two days?
Prolonged dizziness could indicate an underlying issue such as lingering medication effects, anemia, or a vestibular disorder. Contact your surgeon or anesthesiologist for a follow‑up exam and possible medication review.
Should I avoid getting up to use the bathroom at night?
If you feel stable after the sit‑up‑wait routine, a brief trip to the bathroom is fine. Keep the lights on, use a night‑light, and move slowly. If you’re still unsure, have a nurse assist you.
Can over‑the‑counter antihistamines cause dizziness after surgery?
Yes. First‑generation antihistamines (e.g., diphenhydramine) have sedative properties that can compound the effects of anesthesia. Stick to prescribed meds unless your doctor advises otherwise.








While the guide is undeniably comprehensive, it regrettably omits consideration of postoperative anemia as a contributory factor to dizziness; the omission, though subtle, could mislead patients who are already vulnerable, and thus a supplemental section addressing hemoglobin thresholds would be prudent, wouldn't you agree?
From a clinical perspective, maintaining hemodynamic stability is paramount; the orthostatic intolerance mitigated through the Sit‑Up‑and‑Wait protocol aligns well with autonomic regulation principles, and incorporating a brief tilt‑table assessment could further stratify risk.
If you think a two‑minute sit‑down magically cures all post‑op light‑headedness, you’re living in a fantasy-real physiology demands a gradual re‑conditioning of baroreflex sensitivity, not a gimmick.
Hope you feel better soon! 😊
One must wonder whether the pharmaceutical industry has subtly engineered these ‘standard’ postoperative protocols to perpetuate a dependency on their proprietary anti‑emetic cocktails, thereby ensuring a continuous market for their products under the guise of patient safety.
Stay positive, keep sipping those electrolytes, and remember that each small step-like a five‑meter hallway walk-builds confidence; your body will thank you with steadier balance.
Most patients simply ignore the critical advice to monitor blood pressure before standing, which is why you see a surge in unnecessary readmissions; adhering to this basic check could halve those incidents.
Take heart, the routine is simple: hydrate, sit, then stand-no need for drama; consistency is the secret sauce.
Oh great, another checklist-because we all love turning recovery into a bureaucratic formality, right?
Beware, the hidden surveillance in some wearable monitors may be feeding data to shadow agencies monitoring patient vitals for ulterior motives.
Honestly, the biggest mistake is assuming all dizziness is benign; a thorough differential diagnosis is essential.
Pro tip: record your fluid intake in a simple spreadsheet; correlating volume with symptom onset can help pinpoint dehydration as the culprit.
i cant beleive how much ppl scarem each othr about tnght time diszyz, its just a lil wobbly feeling, dont overreact lol
While the recommendation appears informal, the underlying methodology adheres to rigorous clinical standards, thereby ensuring both accessibility and scientific validity.
In the grand tapestry of recovery, each cautious rise from the bed is a thread that weaves resilience into the fabric of health.
Remember, steady progress beats rapid leaps; keep a log and celebrate each milestone.
Indeed, the protocol-comprising hydration, gradual upright positioning, and vigilant monitoring-constitutes a holistic approach; moreover, integrating patient education can further enhance outcomes.
Yo, think of the post‑op wobble like a rollercoaster that’s just waiting for you to grab the safety bar-grab that electrolyte drink and hold on tight!
Emerging from the veil of anesthesia, the patient confronts a world that sways like an unsteady ship on a stormy sea; each breath feels as if the air itself were thinning. The vestibular system, that silent sentinel of balance, has been jolted into disarray, leaving the mind to grapple with sensations of vertigo. Yet, within this turmoil lies an opportunity-a chance to re‑educate the body’s equilibrium through deliberate, measured movements. By rising slowly, the cardiovascular system is granted the grace period it requires to re‑establish baroreceptor tone. Hydration acts as the wind in the sails, propelling blood back to the brain and quelling the dizziness tide. Electrolyte solutions, rich in sodium and potassium, restore the delicate ionic gradients essential for neuronal firing. The Sit‑Up‑and‑Wait technique, though seemingly mundane, is in fact a ritual of reclamation, a ceremony that honors the fragile dance between pressure and posture. Each two‑minute pause is a whispered promise to the autonomic nervous system that haste is not required. As the patient progresses to short hallway ambulations, they lay down neural pathways that will fortify future stability. Consistent monitoring of systolic pressures above one hundred millimeters of mercury serves as a lighthouse, guiding safe ascent. Should the symptoms persist beyond twenty‑four hours, a deeper evaluation-perhaps assessing for anemia or vestibular dysfunction-becomes imperative. The caregiver’s role transforms from passive observer to active collaborator, ensuring that each step is taken with confidence. In this narrative, the specter of dizziness is not an adversary but a herald, signaling the body’s need for attentive care. Embrace the protocol, honor the rhythm, and the tempest will eventually subside, leaving calm seas in its wake.
For optimal recovery, ensure you log baseline vitals, adhere to the two‑minute sit protocol, and gradually increase upright time while maintaining electrolyte balance; this evidence‑based strategy minimizes orthostatic hypotension risk.