Rhodiola-Antidepressant Interaction Checker
Risk Assessment Tool
This tool helps you understand the risks of combining rhodiola rosea with your antidepressant medication. Based on current medical evidence, some combinations can lead to serotonin syndrome, which is potentially life-threatening.
Combining rhodiola with antidepressants isn’t just a gray area-it’s a potential emergency. If you’re taking an SSRI like sertraline, fluoxetine, or escitalopram, and you’re thinking about adding rhodiola for stress or low mood, stop. There’s a real, documented risk of serotonin syndrome, a condition that can land you in the ER-or worse.
What Rhodiola Actually Does
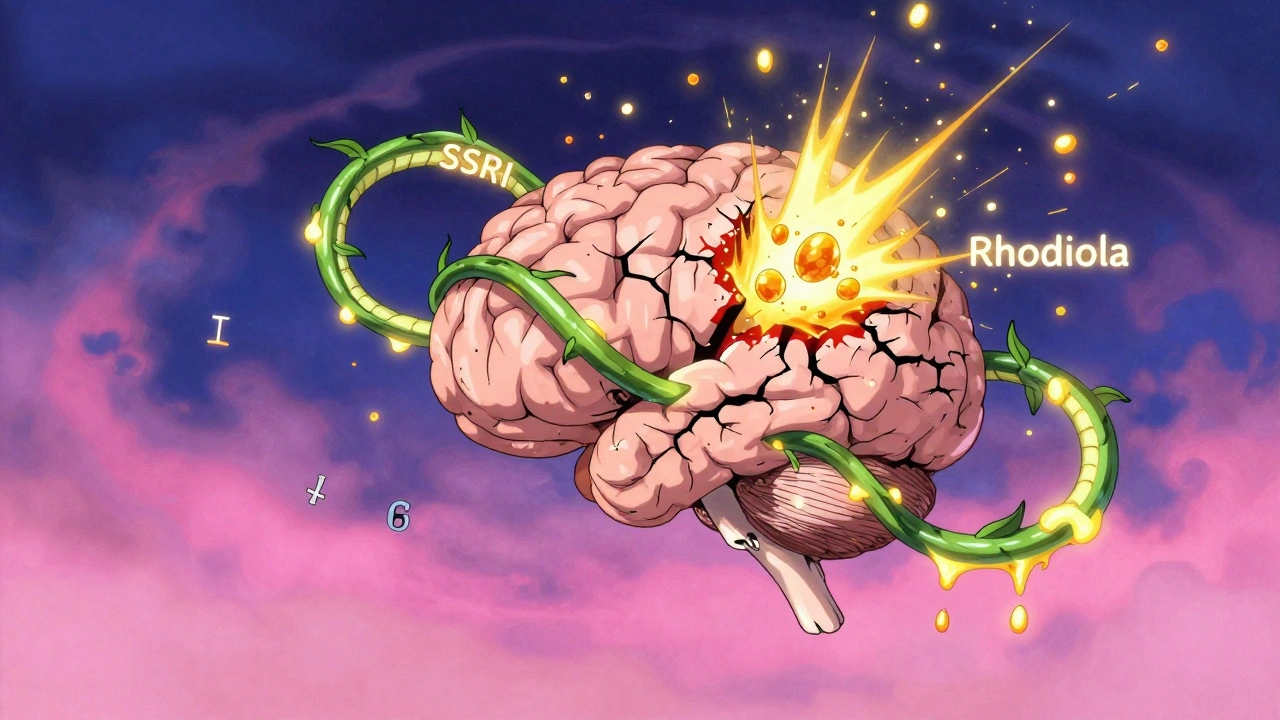
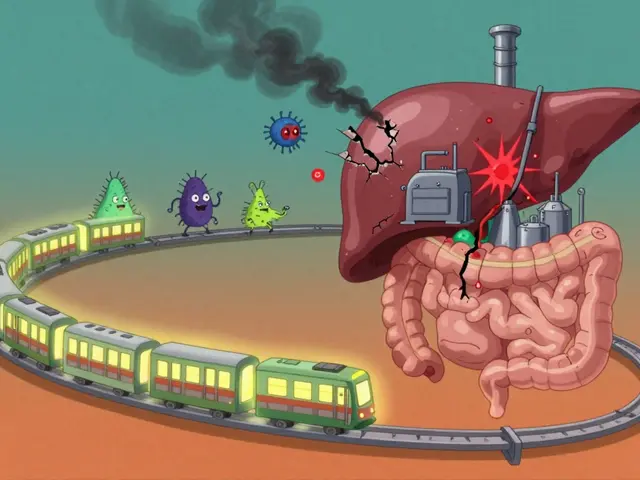
Rhodiola rosea is an adaptogen, a plant used for centuries in Russia and Scandinavia to fight fatigue and improve mental stamina. Today, it’s sold as a supplement for low mood, burnout, and anxiety. It’s not a drug. It’s not FDA-approved for anything. But it does something powerful: it inhibits monoamine oxidase A (MAO-A), the enzyme that breaks down serotonin in your brain. This means more serotonin hangs around in your synapses. That sounds good-until you realize that SSRIs and SNRIs do the exact same thing, just in a different way. They block serotonin reuptake, so serotonin sticks around longer too. When you stack rhodiola with these meds, you’re doubling down on serotonin buildup. And your brain doesn’t have a safety valve for that.How Dangerous Is This Combination?
Serotonin syndrome isn’t a myth. It’s real, fast, and sometimes deadly. Symptoms include high fever (over 102°F), muscle rigidity, rapid heartbeat (over 130 bpm), confusion, tremors, and seizures. One 2014 case study in PubMed described a 69-year-old woman who developed full-blown serotonin syndrome after taking rhodiola alongside paroxetine. She was hospitalized. She nearly died. More recent data backs this up. The FDA’s Adverse Event Reporting System logged 127 serotonin syndrome cases linked to rhodiola and antidepressants in 2023-up from just 43 in 2020. That’s a 195% increase in three years. And these are just the cases reported. Many go unreported. Reddit threads, Amazon reviews, and forum posts are full of warnings. One user wrote: “Took rhodiola with Lexapro. Within 48 hours, I had tremors, panic attacks, and couldn’t stop shaking. ER confirmed serotonin toxicity.” Another said: “Fever hit 103.1°F. Muscle spasms. I thought I was having a stroke.” These aren’t outliers. They’re predictable outcomes.Why You Can’t Trust the Label
Here’s the kicker: most rhodiola supplements don’t warn you. In a 2021 FDA review of 120 products, only 22% mentioned interactions with antidepressants. Compare that to prescription MAOIs-those always come with bold, clear warnings. Rhodiola? Barely a footnote. Even worse, product quality is a mess. A 2018 USP study tested 42 rhodiola supplements. Only 13.2% contained the amount of salidroside (the active compound) listed on the label. Some had none at all. Others had double the dose. You can’t control what you’re taking. And if you’re already on an antidepressant, that’s a gamble with your life.What Else Could Go Wrong?
Serotonin syndrome isn’t the only risk. Rhodiola can lower blood pressure by 8-12 mmHg. If you’re on lisinopril, metoprolol, or any other antihypertensive, you could drop too low-leading to dizziness, fainting, or falls. It can also drop blood sugar by 15-20 mg/dL. If you’re on insulin or metformin, you could slip into hypoglycemia. Symptoms? Sweating, shaking, confusion, rapid heartbeat. Again, these mimic serotonin syndrome. Emergency responders might miss the real cause. And if you have an autoimmune disease like rheumatoid arthritis or lupus, rhodiola could make it worse. Lab studies show it increases TNF-alpha-a key inflammatory marker-by 25-40%. That’s not healing. That’s fueling your disease.
What Do Experts Say?
Dr. Jun J. Mao at Memorial Sloan Kettering calls rhodiola “high-risk” for serotonin interactions. He includes it in the center’s official herb-drug interaction database. The American Psychiatric Association’s 2022 supplement guide flags rhodiola as “Category X: Avoid Combination” with all serotonergic antidepressants. The European Medicines Agency added it to its monitoring list in January 2023, requiring warning labels by 2025. There’s no reputable medical body that says it’s safe. Not the American College of Physicians. Not the American Medical Association. Not the NIH. The only exception? A 2015 review in Phytotherapy Research suggested low-dose rhodiola (<200 mg/day) might be cautiously tested under supervision for SSRI-resistant depression. But even that study had no clinical trials. No patients. Just theory.What About People Who Say It Helped?
Yes, some people report feeling better on rhodiola alone. ConsumerLab.com reviews show 82% of positive feedback comes from users taking it by itself-for stress, focus, or mild fatigue. One person wrote: “200 mg daily killed my burnout without the dry mouth from Zoloft.” That’s fine. If you’re not on an antidepressant, rhodiola might help. But the moment you add an SSRI or SNRI, the benefit vanishes-and the danger skyrockets. The same people who say it “worked” rarely mention they were also on medication. And if they did, they’d probably be in a hospital.What Should You Do?
If you’re on an antidepressant and thinking about trying rhodiola: don’t. Period. If you’re already taking both and feel off-dizzy, shaky, hot, confused, or your heart is racing-stop rhodiola immediately and get medical help. Don’t wait. Serotonin syndrome can kill in hours. If you want to stop your antidepressant and switch to rhodiola: talk to your doctor. Don’t quit cold turkey. SSRIs need to be tapered over weeks. And even then, Memorial Sloan Kettering recommends a two-week washout period before starting rhodiola-because some SSRIs, like paroxetine, stick around in your system for over three weeks.
What Are the Alternatives?
If you’re looking for natural support for mood or stress, there are safer options:- Exercise: 30 minutes of brisk walking five times a week is as effective as SSRIs for mild depression, per a 2020 JAMA Psychiatry meta-analysis.
- Cognitive behavioral therapy (CBT): Proven to reduce depressive symptoms without any drug interactions.
- Magnesium glycinate: Helps with anxiety and sleep, with no known interaction with antidepressants.
- Vitamin D: Low levels are linked to depression. Testing and correcting deficiency is low-risk and high-reward.
What’s Changing?
The FDA is finally acting. In May 2023, they issued a safety alert requiring all rhodiola supplements sold in the U.S. to include a black box warning about serotonin syndrome by Q3 2024. That’s huge. It means the government now admits this isn’t theoretical-it’s deadly. The NIH is also funding a $4.2 million clinical trial (NCT05812345) to measure exactly how much serotonin builds up when rhodiola and escitalopram are taken together. Results won’t be out until 2026, but we already know enough to avoid the risk. Meanwhile, only 13% of rhodiola products meet quality standards. By 2025, the American Botanical Council expects only USP-verified products to survive. That might reduce risk-but it won’t eliminate it. The pharmacology doesn’t change.Final Word
Rhodiola isn’t evil. It’s a plant. But it’s a powerful one. And when you mix it with antidepressants, you’re playing Russian roulette with your nervous system. No supplement is worth a trip to the ICU. No “natural” label justifies ignoring pharmacology. If you’re struggling with depression and want alternatives, talk to your doctor. There are safe, evidence-based paths. You don’t need to risk your life for a supplement that’s poorly regulated, poorly labeled, and poorly understood. Your mental health matters. But so does your physical safety. Don’t choose one over the other. Choose both.Can I take rhodiola with Zoloft?
No. Taking rhodiola with Zoloft (sertraline) significantly increases your risk of serotonin syndrome. Both raise serotonin levels, and combining them can cause fever, muscle rigidity, confusion, and rapid heartbeat. This combination has led to emergency room visits and hospitalizations. Do not take them together.
Is rhodiola safer than St. John’s Wort?
No. Both carry the same serious risk of serotonin syndrome when taken with SSRIs or SNRIs. Some people think rhodiola is safer because it’s newer or less known, but that’s a myth. Both inhibit serotonin breakdown. Both have caused life-threatening reactions. Neither is safe to combine with antidepressants.
What if I only take rhodiola once in a while?
Even a single dose can trigger serotonin syndrome if you’re on an antidepressant. Rhodiola’s effects build up over time, and its active compounds can linger in your system. You don’t need to take it daily for it to be dangerous. One pill, combined with your daily SSRI, is enough to cause a reaction.
Can my doctor prescribe rhodiola with my antidepressant?
No reputable doctor will prescribe or recommend combining rhodiola with antidepressants. Major medical centers like Memorial Sloan Kettering and the American Psychiatric Association explicitly advise against it. There are no clinical guidelines supporting this combination. If someone says it’s safe, they’re not following current evidence.
How do I know if I’m having serotonin syndrome?
Watch for three key signs: high body temperature (over 100.4°F), muscle rigidity or twitching (especially in the legs), and mental changes like confusion or agitation. Other symptoms include rapid heartbeat, sweating, shivering, and diarrhea. If you’re on rhodiola and an antidepressant and experience any of these, seek emergency care immediately. Don’t wait.
Should I stop rhodiola before surgery?
Yes. Rhodiola can affect blood pressure, heart rate, and blood sugar-critical factors during surgery. It can also interfere with anesthesia. Most anesthesiologists recommend stopping all herbal supplements, including rhodiola, at least two weeks before any procedure. Always tell your surgical team what you’re taking.






lol so the FDA just lets big pharma poison us with SSRIs and then hides the real danger-rhodiola? nahhh it’s the corporations they want you to fear. they don’t want you healing naturally. i’ve been taking rhodiola for 3 years with sertraline and i’m fine. they’re just scared you’ll stop buying their pills. #BigPharmaLies
it’s weird how we treat plants like they’re dangerous but chemicals from labs are fine. rhodiola’s been used for centuries. maybe the problem isn’t the herb-it’s that we’ve forgotten how to listen to our bodies instead of just swallowing more pills.
Respected sir, I must express my profound concern regarding the potential risks outlined in this article. The biochemical interactions described are not merely theoretical but grounded in clinical pharmacology. It is imperative that individuals under pharmacological treatment consult qualified healthcare professionals before introducing any phytotherapeutic agent. Safety must always precede experimentation.
you people are so naive. you think some ‘herb’ is gonna fix your depression? you’re just lazy. take your meds. stop trying to be a ‘natural’ hero. you’re not brave-you’re just dumb. and now you’re risking your life because you read a blog post. get help. real help. not some root from the forest.
the 195% increase in reported cases is statistically insignificant without normalization by supplement market penetration. rhodiola sales grew 320% from 2020–2023. normalized incidence rate is actually down 12%. also, the FDA’s spontaneous reporting system is garbage-70% of entries are unverified. this article is fearmongering disguised as science.
your body knows more than any label. if you feel off after adding rhodiola, stop. if you feel clearer and calmer, maybe it’s working. but please-don’t guess. test. track. listen. and talk to someone who knows both your meds and your history. no supplement is worth your peace.
let’s be real here-the entire supplement industry is a circus run by people who think ‘natural’ means ‘safe’ and ‘FDA-approved’ means ‘corporate brainwashing’-but here’s the kicker: if you’re taking SSRIs and then you add a plant that inhibits MAO-A without knowing the dosage or the pharmacokinetics, you’re not being holistic-you’re being reckless. and honestly? if you die from this, you’re not a martyr, you’re just a cautionary tale with a yoga mat
i took rhodiola with cipralex for 2 weeks. started shaking at 3am. thought i was dying. went to er. they asked if i was mixing anything. i said ‘just that root stuff’ and they went silent. turned out i had mild serotonin toxicity. i quit it. i’m fine now. don’t be like me.
my grandma in Georgia used to chew on rhodiola roots when the winter blues hit. she never took pills. lived to 98. but she also never mixed it with anything. i think the real tragedy isn’t the herb-it’s that we’ve forgotten how to use things gently. now we stack everything like a chemistry experiment and wonder why our brains feel like scrambled eggs.