By 2025, the World Health Organization’s goal to eliminate hepatitis C as a public health threat is within reach-but only because of one drug: sofosbuvir. Before its arrival in 2013, hepatitis C treatment meant months of injections, brutal side effects, and cure rates that barely broke 50%. Today, a 12-week course of sofosbuvir-based therapy cures more than 95% of patients, with few side effects and no needles. This isn’t just progress. It’s a revolution.
What sofosbuvir actually does
Sofosbuvir is a direct-acting antiviral (DAA). It doesn’t boost your immune system or fight the virus indirectly. It targets the hepatitis C virus’s RNA polymerase enzyme-the exact tool the virus uses to copy itself. Block that enzyme, and the virus can’t multiply. The virus doesn’t adapt quickly to sofosbuvir, which is why resistance is rare. In clinical trials, fewer than 2% of patients developed resistance, even after treatment failure.
It’s always used in combination with other drugs-like velpatasvir, ledipasvir, or daclatasvir-because hepatitis C has multiple genotypes. A single drug won’t cover them all. But when paired correctly, sofosbuvir turns what was once a lifelong infection into a curable condition. For genotype 1, the most common in the U.S. and Europe, sofosbuvir/ledipasvir cured 97% of patients in real-world studies. For genotype 3, which used to be harder to treat, sofosbuvir/velpatasvir achieved cure rates above 95% even in patients with cirrhosis.
How sofosbuvir changed elimination strategies
Before sofosbuvir, hepatitis C elimination was a fantasy. Treatment was too expensive, too long, and too hard on the body. Only people with advanced liver damage got treated. Most infected individuals never even knew they had it. The virus spread silently in hospitals, prisons, and among people who inject drugs.
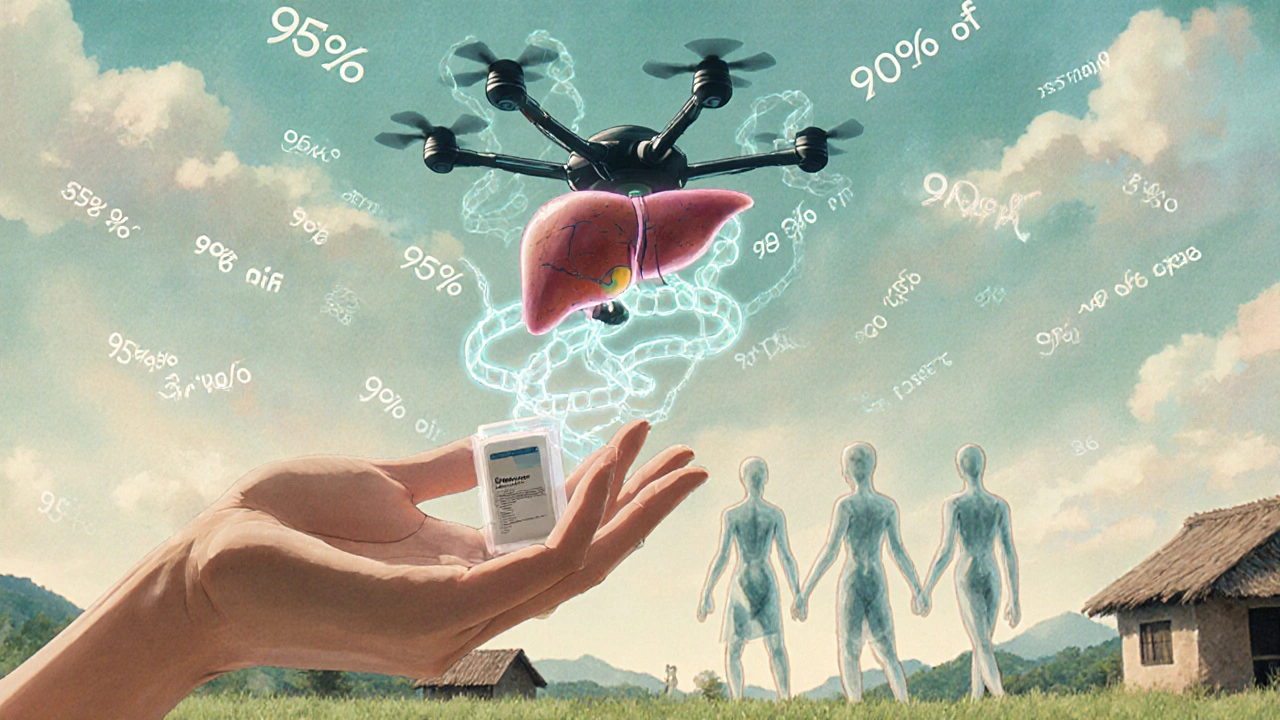
Sofosbuvir flipped the script. Because it’s so effective and well-tolerated, health systems could shift from treating only the sickest to testing and treating everyone who tests positive. Countries like Egypt and Georgia launched nationwide screening campaigns. In Egypt, they tested over 50 million people in three years. Those who tested positive got treatment within weeks. By 2023, Egypt reduced hepatitis C prevalence by 80%. Georgia cut new infections by 90% in five years.
This is the core of elimination: treat early, treat widely, treat simply. Sofosbuvir made that possible. No more monthly clinic visits. No more blood tests every two weeks. Just a daily pill. A 12-week course. Done.
The cost barrier-and how it was broken
When sofosbuvir launched in 2013, a full course cost $84,000 in the U.S. The price sparked global outrage. But the real story isn’t the sticker price-it’s what happened next.
Generic manufacturers in India, Egypt, and Bangladesh started producing sofosbuvir under voluntary licenses. By 2017, a full 12-week course of generic sofosbuvir + velpatasvir cost as little as $45 in low-income countries. The Global Fund, UNITAID, and Médecins Sans Frontières used these generics to scale treatment across Africa and Asia. In Ukraine, a national program treated 120,000 people between 2018 and 2022 using generics priced under $100 per patient.
Even in high-income countries, pressure from patient groups and public health advocates forced price reductions. The UK’s NHS began negotiating bulk deals, bringing the cost per patient down to under £500 by 2020. Today, most high-income nations have treatment programs where cost is no longer the main barrier-it’s finding people who don’t know they’re infected.

Who’s still being left behind
Despite the breakthroughs, hepatitis C hasn’t been eliminated everywhere. In the U.S., only about 30% of people with hepatitis C have been diagnosed, and even fewer have been treated. Why? Stigma. Lack of access. Fragmented healthcare.
People who inject drugs, incarcerated individuals, and homeless populations are the hardest to reach. Many clinics won’t treat them unless they’re sober or housed. But studies show that treating people while they’re still using drugs works just as well. In fact, one study in San Francisco found that offering treatment inside needle exchange programs increased cure rates by 40% compared to traditional clinics.
Prisons are another missed opportunity. Over 1 in 10 inmates in the U.S. have hepatitis C. Yet only 1 in 5 receive treatment. Countries like Australia and Canada have shown that treating prisoners not only saves lives-it stops transmission when they’re released.
The path forward: testing, linking, treating
The next phase of hepatitis C elimination isn’t about better drugs. It’s about better systems.
First, testing. Blood tests for hepatitis C are cheap, fast, and can be done with a finger prick. Community pharmacies, mobile vans, and even home test kits are now available. In Scotland, pharmacies now offer free hepatitis C tests alongside flu shots. Over 10,000 people were tested in one year. One in 50 tested positive-and most had no idea.
Second, linking. Once someone tests positive, they need to be connected to care immediately. Too often, people get a positive result and vanish from the system. Peer navigators-people who’ve been through treatment themselves-help bridge that gap. In New York City, peer navigators increased treatment initiation by 65% among people who use drugs.
Third, treating. Treatment must be simple, fast, and stigma-free. No more waiting for liver damage. No more mandatory counseling. Just test, confirm, prescribe, and follow up in 12 weeks. That’s it.
What’s next after sofosbuvir
Sofosbuvir isn’t the end of the road-it’s the foundation. New combinations are being tested: pibrentasvir/glecaprevir, for example, works in just 8 weeks for most genotypes. Some trials are even exploring 4-week regimens.
But the real innovation isn’t in the pills. It’s in delivery. In Rwanda, drones deliver test kits to remote villages. In Brazil, AI tools scan hospital records to flag patients who haven’t been tested. In Canada, community health workers carry portable labs to Indigenous communities.
What’s clear is this: we have the tools. We have the science. We have the cure. What we need now is the will to reach everyone.
Can sofosbuvir cure hepatitis C in all genotypes?
Yes, when used in the right combination. Sofosbuvir works against all six major genotypes of hepatitis C. But it’s never used alone. For genotype 1, it’s paired with ledipasvir or velpatasvir. For genotype 3, velpatasvir is preferred. For genotype 4, 5, and 6, sofosbuvir/velpatasvir is the standard. Cure rates are consistently above 95% across all genotypes when the correct combination is used.
Is sofosbuvir safe for people with kidney disease?
Yes, but with caution. Sofosbuvir is cleared mostly by the kidneys, so people with severe kidney impairment (eGFR below 30) need a different regimen. The combination of sofosbuvir and velpatasvir is approved for use in patients with advanced kidney disease, including those on dialysis. Other combinations, like sofosbuvir/ledipasvir, are not recommended in this group. Always check kidney function before starting treatment.
Can you get hepatitis C again after being cured with sofosbuvir?
Yes. Being cured doesn’t make you immune. If you’re exposed again-through sharing needles, unsafe medical procedures, or unsterile tattoos-you can become infected again. That’s why harm reduction and ongoing testing are critical, especially for people who continue to inject drugs. Cure is not protection. Prevention is still needed.
How long does it take to know if sofosbuvir worked?
Twelve weeks after finishing treatment, a blood test checks for the presence of hepatitis C virus RNA. If the virus is undetectable at that point, you’re considered cured. This is called a sustained virologic response (SVR12). Studies show that over 99% of people who achieve SVR12 remain virus-free for life. No further testing is needed unless there’s a new exposure.
Are there any long-term side effects of sofosbuvir?
No. Clinical data from over 100,000 treated patients shows no long-term side effects from sofosbuvir-based regimens. Short-term side effects-like mild fatigue or headache-usually disappear within days of finishing treatment. Liver function improves in almost all patients after cure, and the risk of liver cancer drops significantly. For people with cirrhosis, cure reduces the chance of liver failure by 70% over 10 years.
Final thoughts: elimination is possible
There are still 58 million people living with hepatitis C worldwide. But we now have the tools to end this epidemic. Sofosbuvir didn’t just change treatment-it changed what we believe is possible. We can cure the virus. We can stop transmission. We can eliminate hepatitis C in our lifetimes. The only thing left to do is make sure no one is left behind.







Yeah sure, cure rate 95%... until you realize the pill costs more than my car. Glad someone in India made it cheap so the rest of us can live. Thanks, generic manufacturers. Not the pharma bros.
People still get hepatitis C? Like... how? Did they not learn from the 90s? My cousin did a tattoo in a garage and now she's 'cured' but still smokes crack. So what's the point?
Revolution? More like a marketing stunt wrapped in clinical data. We fix symptoms, not systems. And yes, I know what DAA means. You don't need to explain.
They cured the virus but not the human condition. We treat people like broken machines. We don't fix the loneliness, the poverty, the shame that lets hepatitis C spread. Sofosbuvir is a Band-Aid on a bullet wound.
Look, I get it, the drug works. But let’s not pretend this is some humanitarian triumph. Big Pharma made billions. Then, when the generics came in, they cried and sued and lobbied. And now we’re supposed to clap because a pill costs $45 instead of $84K? That’s not progress-that’s damage control. And don’t even get me started on how the U.S. still won’t treat people who use drugs unless they’re ‘clean.’ Like, you want them cured? Then stop treating them like criminals. It’s not rocket science. It’s basic decency. And yet here we are, letting people die because we’re too proud to admit we failed them.
Interesting how Egypt did it right. Tested 50 million people. No drama. No stigma. Just pills and patience. Meanwhile, we’re still arguing over whether to treat addicts. I mean… what even are we?
Good to know the science works. Hope more countries follow Egypt.
You think this is about health? It’s about control. The moment you make treatment simple and cheap, you empower people. And empowered people don’t stay quiet. They ask why their housing is bad. Why their food is poisoned. Why their prisons are full. Sofosbuvir didn’t cure hepatitis C-it exposed the rot underneath. And now they’re scared.
It’s funny how we celebrate the pill but ignore the person taking it. The guy in the alley. The woman in the shelter. The kid who got it from a contaminated needle at 14. The cure is there. But we still act like they’re invisible.
One thing often missed: curing hepatitis C reduces liver cancer rates by 70% over a decade. That’s not just personal health-it’s economic. Fewer transplants, fewer ICU stays, fewer families broken. This isn’t charity. It’s smart public finance.
Thank you for this deeply thoughtful and meticulously researched piece. It is truly inspiring to witness the power of medical innovation paired with compassionate policy implementation. I hope we continue to prioritize equitable access, as the moral imperative is undeniable. 🌍❤️
Why are we giving free pills to criminals? We should be deporting them, not curing them.
So you're telling me a NS5B polymerase inhibitor with a half-life of 27 hours and a high barrier to resistance can achieve SVR12 in >95% across genotypes? That’s not a miracle, that’s pharmacokinetic engineering at its finest. The real win? The DAA combo avoids interferon’s cytokine storm. Game changer.
This gave me hope 😭👏👏👏
Imagine if we treated addiction like we treat hepatitis C-no judgment, no waiting, just help. No one gets turned away because they’re not ‘ready.’ No one has to hit rock bottom before they get a shot. That’s the real cure. Not the pill. The mindset.