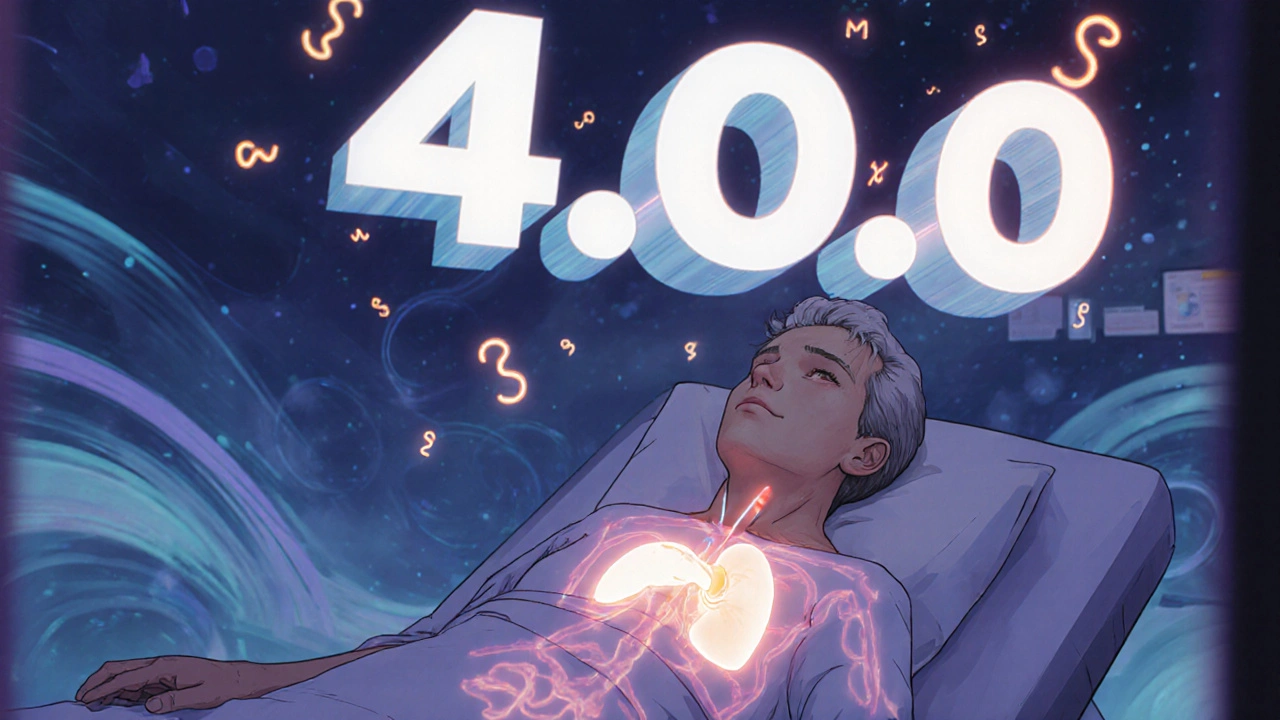
When your TSH is high but your thyroid hormone levels are normal, you’re not necessarily sick. But should you take medicine anyway? That’s the question millions of people face every year after a routine blood test shows an elevated TSH. Subclinical hypothyroidism isn’t a disease you can feel in your bones-it’s a number on a lab report. And that number, between 4.0 and 10.0 mIU/L, is where the real debate begins.
What Exactly Is Subclinical Hypothyroidism?
Subclinical hypothyroidism means your thyroid-stimulating hormone (TSH) is higher than normal, but your free T4 (thyroxine) is still in the normal range. Your pituitary gland is sending out more TSH because it’s trying to get your thyroid to produce more hormone. But your thyroid is still holding up-for now. This isn’t full-blown hypothyroidism. You don’t have the classic symptoms like extreme fatigue, weight gain, or dry skin. At least, not always.
It’s surprisingly common. About 1 in 5 adults in the U.S. have elevated TSH at some point. The older you are, the more likely it is. Up to 20% of women over 60 show signs of it. But here’s the catch: not everyone with a high TSH will ever develop full hypothyroidism. Some stay like this for decades without change.
The diagnosis isn’t based on one test. You need two elevated TSH readings, taken 2 to 3 months apart. Why? Because stress, illness, medications, or even a bad night’s sleep can temporarily bump up TSH. One high number doesn’t mean you need lifelong pills.
When Does High TSH Actually Need Treatment?
The biggest question doctors face: Should you treat TSH levels between 4.0 and 10.0 mIU/L? The answer isn’t the same for everyone.
Most major guidelines agree on one thing: if your TSH is above 10.0 mIU/L, treatment with levothyroxine is usually recommended. The risk of progressing to full hypothyroidism jumps to 70% within four years. Plus, higher TSH levels are linked to higher cholesterol, increased heart disease risk, and possible cognitive changes over time.
But what about TSH between 5 and 10? That’s the gray zone. Here’s where things get messy.
The American Thyroid Association says: wait. Only treat if TSH is above 10. The Endocrine Society says: consider treatment if you’re under 50, have symptoms, or have thyroid antibodies. The American Association of Clinical Endocrinologists says: start thinking about treatment at TSH 7 or higher. And the Royal Australian College of General Practitioners says: don’t treat at all unless it’s above 10.
Why the disagreement? Because the science is mixed.
A 2017 study in JAMA followed 737 older adults with TSH between 4 and 10. They gave half levothyroxine. After a year, there was no difference in energy, mood, or quality of life. The other group, untreated, did just fine.
But another study in Thyroid in 2020 found that people under 50 with TSH 7-10 and positive thyroid antibodies had a 32% reduction in fatigue and brain fog after starting low-dose levothyroxine.
So what’s the real difference? It’s not just the number. It’s who you are.
Who Benefits Most from Treatment?
If you’re under 50, have symptoms, and your thyroid antibodies are positive-you’re in the high-risk group. Thyroid peroxidase (TPO) antibodies mean your immune system is attacking your thyroid. That’s Hashimoto’s, even if it’s early. People with positive antibodies are 2.3 times more likely to progress to full hypothyroidism. For them, early treatment isn’t just about feeling better-it’s about stopping the disease in its tracks.
Women planning pregnancy should also be treated if TSH is above 2.5-4.0 mIU/L. Even subclinical hypothyroidism can affect fertility and increase miscarriage risk. The American Society for Reproductive Medicine recommends treating pregnant women or those trying to conceive with TSH over 4.0.
People with high cholesterol or heart disease should also be considered for treatment. High TSH can raise LDL cholesterol, and some studies show that lowering TSH improves lipid profiles-even if symptoms don’t change.
But if you’re over 65? The risks of treatment start to outweigh the benefits. A 2021 study found that older adults treated for TSH below 10 had a 12% higher risk of death-not from thyroid problems, but from heart rhythm issues like atrial fibrillation. Levothyroxine can overstimulate an aging heart. For older patients, the goal isn’t to normalize TSH-it’s to avoid harm.
What About Symptoms? Do They Matter?
Many people with elevated TSH feel tired, cold, or foggy. But so do a lot of people without it. Studies show 30-40% of people with normal thyroid function report the same symptoms. That’s because fatigue and brain fog are common. They come from stress, poor sleep, depression, or just aging.
So don’t treat symptoms alone. Use a tool like the Thyroid Symptom Rating Scale or ThyPRO questionnaire. These aren’t just feel-good checklists-they’re validated tools that help separate real thyroid-related symptoms from everything else.
If you’ve scored high on the scale, your TSH is above 7, and your antibodies are positive? Treatment might help. But if your TSH is 5.5, you feel fine, and your antibodies are negative? You’re probably better off watching and waiting.
How Is Treatment Done? And What Are the Risks?
If you and your doctor decide to treat, you’ll start with a low dose: 25 to 50 micrograms of levothyroxine daily. That’s less than half the dose usually given for full hypothyroidism. Your body is still making some hormone-you’re just giving it a nudge.
You’ll get your TSH checked again in 6 to 8 weeks. Dose adjustments are small-usually 12.5 to 25 mcg at a time. The goal isn’t to crush your TSH into the bottom of the range. It’s to get it into the middle: around 1.0 to 3.0 mIU/L.
Too much levothyroxine? That’s dangerous. It can cause bone loss, heart palpitations, and even atrial fibrillation. Especially in older adults. And it’s easy to overdo it. Many people take it with coffee, calcium, or iron supplements-things that block absorption. You need to take it on an empty stomach, at least 30-60 minutes before eating, and wait 4 hours before taking supplements.
And here’s the kicker: you might need to take it for life. Stopping it means your TSH will likely rise again. That’s why the decision to start should be thoughtful-not rushed.
What Should You Do Next?
Don’t panic if your TSH is high. Don’t demand pills either. Do this:
- Get a second TSH test in 2-3 months.
- Ask for thyroid antibody (TPO) testing.
- Check your cholesterol and heart health.
- Rate your symptoms with a simple checklist.
- If you’re a woman planning pregnancy, talk to your doctor now.
- If you’re over 65, ask whether treatment is truly necessary.
Most people with TSH between 5 and 10 don’t need medication. But a small group-those with antibodies, symptoms, or high cardiovascular risk-will benefit.
The key is personalization. Not numbers. Not guidelines. Not fear. It’s your body, your risk, your life.
What’s Coming Next?
Research is shifting. The 2023 American Thyroid Association draft guidelines suggest treating younger patients with TSH above 7 if antibodies are present. New tools are being developed to track TSH velocity-how fast your TSH is rising. A spike of 1 mIU/L per month means you’re much more likely to progress.
Companies like Roche are rolling out calculators that use your past TSH values to predict your risk. This isn’t science fiction-it’s the future of thyroid care.
And one big question remains: are our normal TSH ranges too high? A 2022 study of 27,000 people suggested the upper limit for adults under 50 should be 2.5, not 4.0. If that’s true, then nearly 1 in 3 young adults might be labeled with subclinical hypothyroidism. That could mean millions more people being treated-many of whom don’t need it.
Until then, the safest approach is patience, testing, and personal context-not a one-size-fits-all pill.
Is subclinical hypothyroidism a real condition or just a lab anomaly?
It’s both. Subclinical hypothyroidism is a real biochemical state-an elevated TSH with normal T4. But not everyone with this state will develop symptoms or health problems. For some, it’s a warning sign of future thyroid failure. For others, it’s just a fluctuation. The key is identifying who’s at risk, not treating every high number.
Can I treat subclinical hypothyroidism naturally?
No proven natural treatments exist. Supplements like selenium or iodine won’t lower TSH unless you have a deficiency-and those are rare in the U.S. Diet changes, stress reduction, and sleep help overall health, but they won’t fix an autoimmune thyroid issue. If you have positive antibodies and rising TSH, levothyroxine is the only treatment proven to prevent progression.
Will I need to take thyroid medication forever?
Most people with persistent elevated TSH and positive antibodies will need lifelong treatment. But if your TSH was only mildly high due to illness or stress, and it returns to normal after retesting, you may never need medication. That’s why repeat testing is essential before starting.
How often should I get my TSH checked if I’m not being treated?
If your TSH is between 5 and 10 and you’re not on medication, check it once a year. If it’s above 8 or you have antibodies, check every 6 months. If it’s stable and you’re over 65 with no symptoms, you can stretch to every 2 years. Rapid increases-like jumping from 5 to 8 in 6 months-need faster follow-up.
Can elevated TSH cause weight gain?
Mildly elevated TSH alone rarely causes significant weight gain. Most people with subclinical hypothyroidism gain less than 2-3 pounds, if any. If you’re struggling with weight despite normal T4, look elsewhere-diet, activity, sleep, or hormones like insulin or cortisol are more likely culprits. Treating TSH won’t magically melt extra pounds.






People get so worked up over a number on a lab sheet like it's a death sentence
TSH 5.8? Cool. So am I after three cups of coffee and no sleep
Stop treating labs like gospel and start treating people
Ohhh, so now we're supposed to trust 'guidelines' from a bunch of overpaid endocrinologists who've never held a real job? In America, we don't let bureaucrats decide what's wrong with your body!
My grandfather worked 60 hours a week, raised five kids, and never took a thyroid pill-his TSH was 8.2 and he lived to 94!
They're pushing pills because Big Pharma owns the AMA, the FDA, and your doctor's continuing education budget!
And don't get me started on 'antibodies'-that's just a fancy word for 'your immune system is doing its job'!
Why do we let the medical-industrial complex turn every minor fluctuation into a lifelong drug dependency?
I'm not taking levothyroxine just because some guy in a white coat says so-I'll take my chances with green tea and sunlight!
And if you're telling me that 1 in 3 young adults are 'diseased' because their TSH is above 2.5? That's not medicine-that's mass psychological manipulation!
Wake up, sheeple!
I just found out my TSH was 6.1 last month and I cried for an hour 😭
I mean, I’ve been tired since January, my hair’s falling out, I gained 12 pounds even though I’m eating salad every day…
And now I’m reading this and I’m like… maybe I’m not just lazy??
But then I read the part about older people and heart risks and now I’m terrified to even ask my doctor for a pill 😅
What if I start taking it and then my heart gives out??
What if I DON’T take it and then I get dementia??
WHY IS THIS SO HARD??
Why can’t they just say ‘yes, take it’ or ‘no, don’t’?? Why is everything so… nuanced??
I just want to feel normal again 😔
My doctor said my TSH was 5.4 and told me to wait six months. I did. It went to 5.8. He said still no meds. I asked about antibodies. He said no need unless I’m planning to get pregnant. I’m 32, female, have anxiety and fatigue, and I’m just tired of being told I’m fine when I don’t feel fine.
I got the test done privately. TPO antibodies were high. I started 25 mcg. In two weeks, my brain fog lifted. I slept through the night. I didn’t lose weight, but I stopped gaining.
I’m not saying everyone needs it. But if you feel off and your antibodies are up, don’t wait for your TSH to hit 10.
It’s not a conspiracy. It’s biology.
It is imperative to underscore that the clinical management of subclinical hypothyroidism must be predicated upon a rigorous assessment of individual risk stratification, rather than the application of arbitrary population-based thresholds.
The evidence presented in the JAMA study, while methodologically sound, fails to account for long-term cardiovascular and metabolic sequelae that manifest over decades.
Furthermore, the omission of longitudinal data regarding progression rates in antibody-positive cohorts undermines the validity of a wait-and-see approach in younger populations.
Physicians must exercise clinical judgment, not algorithmic compliance.
Standardization without personalization is not medicine-it is mechanistic dogma.
My doctor ignored my symptoms for two years. Said my TSH was 'just borderline.' I was exhausted, my skin was cracking, I couldn't think straight.
Finally, I found a doctor who listened. TPO antibodies were sky-high. Started levothyroxine. Within three weeks, I cried because I remembered what it felt like to be awake.
Now my husband says I'm 'different.' Like I'm not the same person.
But I'm not the same person because I was dying inside and no one saw it.
They told me it was stress.
They told me I was just getting older.
They told me it was all in my head.
And now I'm alive.
And I'm angry.
Because so many people are still suffering because doctors are too lazy to look past the numbers.
The ontological status of subclinical hypothyroidism is not binary-it exists along a dynamic continuum of immune-metabolic dysregulation.
TSH is a proxy, not a diagnosis. The pituitary-thyroid axis is a feedback loop embedded in circadian, inflammatory, and neuroendocrine networks.
When we reduce it to a number, we collapse complexity into pathology.
But when we ignore the signal because it doesn't fit a guideline, we commit epistemic violence.
The real question isn't whether to treat-it's whether our medical paradigm can tolerate uncertainty.
And if we can't, then we're not healing-we're managing fear.
Bro TSH 5.5 and no symptoms just get a coffee and move on
Why are we making everything a disease
Did you know that the normal TSH range was changed in 2002 because pharmaceutical companies lobbied the AMA to expand the definition of hypothyroidism?
They needed more people to buy levothyroxine.
And now every woman over 40 is being told she's 'diseased' just because her TSH is 5.2.
They even changed the normal range from 0.5–5.0 to 0.4–4.0 so more people could be labeled sick.
And now they want to lower it to 2.5?
This isn't science. This is profit.
They don't want you to feel better-they want you to take a pill forever.
Check your thyroid… but don't trust the system.
Ugh another one of these posts
Just take the pill already
Who cares about guidelines
My friend did and now she's fine
So I'm taking mine too