Every year, millions of people reach for antihistamines and decongestants without a second thought. They’re on every pharmacy shelf, in every medicine cabinet, and often taken without reading the label. But here’s the truth: these common allergy meds carry real, sometimes serious, risks - especially if you’re over 65, have high blood pressure, or are taking other medications. Many people think because it’s over-the-counter, it’s safe. That’s a dangerous assumption.
What antihistamines really do - and what they hide
Antihistamines block histamine, the chemical your body releases during an allergic reaction. That’s why they help with sneezing, itchy eyes, and runny nose. But not all antihistamines are the same. First-generation ones like diphenhydramine (Benadryl) and doxylamine (Unisom) cross the blood-brain barrier. That’s why they make you sleepy - and why they’re so risky for older adults.Up to 60% of people who take first-gen antihistamines feel drowsy. That’s not just inconvenient - it’s dangerous. In adults over 65, this drowsiness increases the risk of falls by 300%, according to AARP. These meds also cause dry mouth, constipation, blurry vision, and trouble urinating. For men with enlarged prostates, that last one can turn into a medical emergency.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are much safer for daily use. They cause drowsiness in only 10-15% of users. But even these aren’t risk-free. They can still raise blood pressure slightly and interact with other drugs. And if you’re pregnant, the American College of Obstetricians and Gynecologists advises sticking to second-gen options only under a doctor’s care.
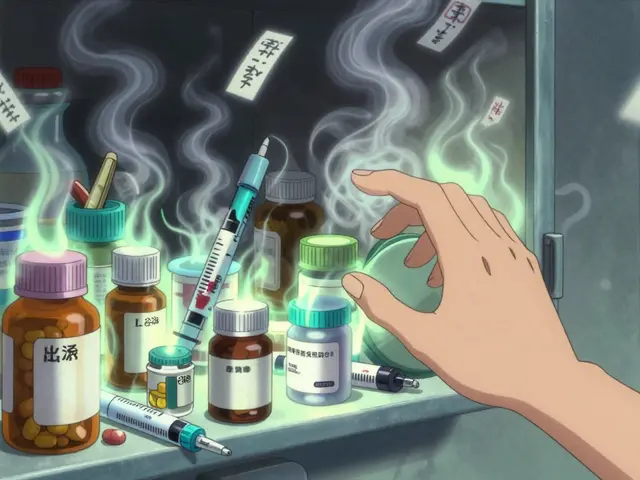
Decongestants: The hidden danger in your medicine cabinet
Decongestants like pseudoephedrine (Sudafed) and phenylephrine shrink swollen blood vessels in your nose. That’s why your stuffy nose clears up fast. But that same vasoconstriction happens everywhere in your body - including your heart and brain.Forty-five percent of users report insomnia. Thirty percent feel nervous or anxious. Fifteen percent get heart palpitations. And for people with high blood pressure? This is where it gets scary. Mayo Clinic says decongestants can raise systolic blood pressure by 5-10 mmHg. That might not sound like much - but for someone already at 150/90, that push could trigger a stroke or heart attack.
Then there’s the nasal spray trap. Products like oxymetazoline (Afrin) give quick relief - but if you use them longer than three days, you get rebound congestion. That’s right: your nose gets more blocked than before. Half of users who go past the three-day limit end up stuck in a cycle of dependence.
Combination meds: The silent overdose risk
You’ve seen them: “All-in-one” cold and allergy formulas. They promise to fix everything - congestion, cough, fever, pain. But they’re a minefield.According to the FDA, 68% of these combo products contain multiple active ingredients. That means you could be taking two different antihistamines at once - or doubling up on acetaminophen. And acetaminophen? Too much of it - over 4,000 mg a day - can cause liver failure. You don’t need to take extra Tylenol. Just one of these combo pills might already bring you close to the limit.
Worse, many people don’t realize they’re taking multiple drugs. They take a decongestant for congestion, then grab a nighttime cold tablet for sleep - and end up with two antihistamines and two decongestants in their system. That’s how emergency rooms see so many cases of rapid heart rate, seizures, and confusion - especially in kids under two. The FDA has banned OTC cough and cold meds for children under two because of 123 reported deaths between 1969 and 2006.

Who should NEVER take these meds
If you have any of these conditions, you need to talk to a doctor before touching an antihistamine or decongestant:- High blood pressure
- Heart disease or irregular heartbeat
- Enlarged prostate
- Glaucoma (especially angle-closure)
- Diabetes
- Thyroid problems
- Liver or kidney disease
The NHS and Mayo Clinic both say: don’t use decongestants if you have any of these. And for antihistamines? The American Geriatrics Society’s Beers Criteria lists first-gen ones like diphenhydramine as “potentially inappropriate” for older adults. Why? Because they’re anticholinergic - they mess with brain chemicals linked to memory and alertness. In seniors, this can lead to confusion, hallucinations, and even dementia-like symptoms.
Deadly interactions you didn’t know about
The biggest risk isn’t the medicine itself - it’s what you mix it with.Decongestants and antidepressants? Dangerous. Taking pseudoephedrine with an SSRI or MAOI can spike blood pressure to over 180 mmHg - a hypertensive crisis. That’s a medical emergency.
Antihistamines and alcohol? Double the drowsiness. That’s why older adults who take Benadryl and have a glass of wine at dinner are five times more likely to fall.
Energy drinks and decongestants? A bad combo. Caffeine and pseudoephedrine both stimulate your nervous system. Together, they can cause palpitations, anxiety, and even heart rhythm problems. Rutgers University’s Poison Control Center saw a 25% jump in calls about this mix in 2022.
And don’t forget: if you’re on MAOIs (a type of antidepressant), you must wait two full weeks after stopping them before using any decongestant. The interaction can be fatal.

What to do instead
You don’t need to suffer. There are safer options.For congestion, try a saline nasal spray. It’s just salt water - no side effects, no rebound congestion. For chronic stuffiness, intranasal corticosteroids like fluticasone (Flonase) are more effective than decongestants and don’t raise blood pressure.
For allergies, second-gen antihistamines are your best bet. They work just as well as the old ones - without the brain fog. And if symptoms last more than 10-14 days? That’s not an allergy. That’s a sinus infection, or something else. Mayo Clinic says it’s time to see a provider.
Pharmacists are your secret weapon. The American Pharmacists Association says 78% of OTC medication problems could be avoided with a simple chat at the counter. Ask them: “Is this safe for me, given what else I’m taking?”
When to stop and call your doctor
Stop taking these meds and get help if you experience:- Chest pain or irregular heartbeat
- Severe headache or blurred vision
- Difficulty urinating
- Confusion, hallucinations, or seizures
- Swelling of the face, lips, or tongue
And if you’ve been using an OTC allergy med for more than two weeks without improvement - you’re not fixing the problem. You’re masking it. And that’s when real damage can start.
Can I take antihistamines every day?
Second-generation antihistamines like loratadine or cetirizine are generally safe for daily use if your allergies are chronic. But first-generation ones like diphenhydramine are not - they build up in your system and increase side effects over time. Always check with your doctor if you need daily medication for more than a few weeks.
Are decongestants safe for people with high blood pressure?
No. Decongestants like pseudoephedrine and phenylephrine can raise blood pressure, sometimes dangerously. Even if your pressure is controlled, these meds can undo that. The NHS and Mayo Clinic both warn against their use in people with hypertension. Saline sprays or nasal corticosteroids are safer alternatives.
Why is Benadryl bad for older adults?
Benadryl (diphenhydramine) is a first-generation antihistamine with strong anticholinergic effects. It blocks acetylcholine, a brain chemical needed for memory and muscle control. In older adults, this causes confusion, dizziness, constipation, urinary retention, and increases fall risk by 300%. The Beers Criteria lists it as a medication to avoid in people over 65.
Can I use nasal decongestant sprays longer than 3 days?
No. Using nasal sprays like Afrin beyond three days causes rebound congestion - your nose becomes more blocked than before. This happens in about half of users who exceed the limit. It’s not addiction - it’s a physical reaction. If congestion lasts longer than a week, see a doctor. You may need a steroid spray or treatment for sinusitis.
Is it safe to take allergy meds with alcohol?
Not with first-generation antihistamines. Mixing Benadryl or doxylamine with alcohol multiplies drowsiness and impairs coordination. This dramatically increases fall risk, especially in older adults. Even second-gen antihistamines can cause mild drowsiness in some people, so it’s best to avoid alcohol when starting any new allergy med.
What should I do if I accidentally took too much?
Call your local poison control center immediately. In the UK, dial 111; in the US, call 1-800-222-1222. Do not wait for symptoms. Overdosing on antihistamines can cause seizures, heart rhythm problems, or coma. Overdosing on decongestants can cause dangerously high blood pressure, stroke, or heart attack. Time matters.








I used to take Benadryl like candy until my grandma fell and broke her hip. Now I stick to Zyrtec. No more brain fog, no more dizziness. Simple swap, life-changing.
EVERY SINGLE PHARMACY IS PUSHING THESE TOXINS ON US!!! They don't care if you die-they care about their quarterly profits!! You think Big Pharma gives a damn about your prostate? HA!! They're selling you death in a bottle labeled 'ALLERGY RELIEF'!!!
They don't want you to know this-but antihistamines were originally developed during WWII as chemical warfare countermeasures. Yeah. You read that right. The same stuff that makes your nose stop running was designed to paralyze enemy troops. Now it's in your kid's gummy vitamins. Who's really in control here? 🤔
Just got off the phone with my pharmacist and she was like, 'Ma'am, you're taking three things that all say 'do not use with high blood pressure.' 😳 I almost cried. Thank you for this post-seriously, this saved me. 🙏
Interesting breakdown. I’ve been using Flonase for years and never realized how much safer it is than Sudafed. I used to feel like a jittery ghost after decongestants. Now I just spray and breathe. No drama.
US people are so weak. In Australia, we just tough it out. If your nose is stuffed, drink a beer and sleep it off. No meds needed. All this 'risk' talk is just fearmongering.
As a nurse who's seen patients in the ER after mixing OTC meds with antidepressants-I cannot stress this enough: YOU ARE NOT A RESEARCH SUBJECT. Read the label. Ask the pharmacist. If you're unsure, DON'T TAKE IT. Your life isn't worth the gamble.
People who take Benadryl every night to sleep are just trading one addiction for another. You think you're helping yourself-but you're slowly erasing your memory, one pill at a time. Wake up. Your brain is not a vending machine.
My dad’s 72 and takes Claritin daily. No issues. He also drinks coffee, walks 5 miles a day, and doesn’t take anything else. Maybe the problem isn’t the meds-it’s everything else going on in your body.
They say 'just ask your pharmacist' like it's that easy. But what if your pharmacist is overworked, underpaid, and rushing you through the line like you're a grocery item? What if they don't even know the interaction between your blood pressure med and that little blue pill? We're not just ignoring risks-we're living in a system that *designed* us to ignore them.