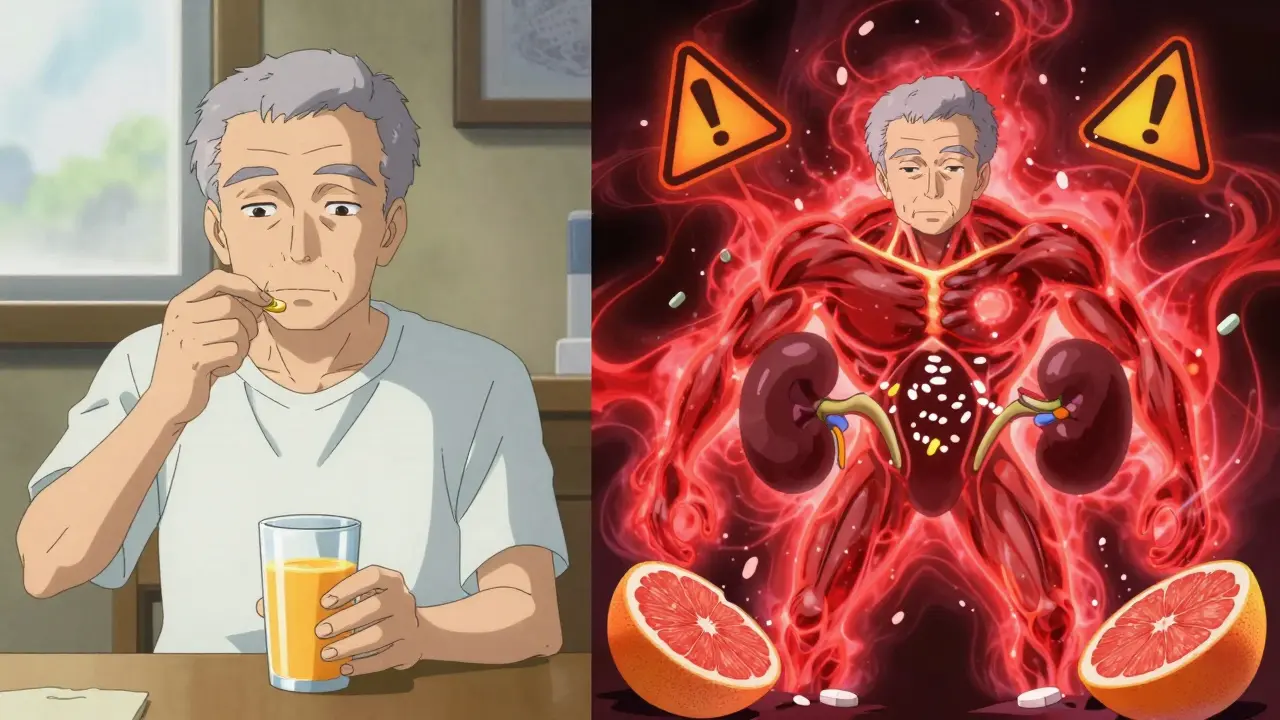
One glass of grapefruit juice in the morning might seem like a healthy habit-until it turns dangerous. For people taking certain medications, this citrus drink isn’t just a harmless breakfast addition. It can turn a safe dose into a toxic one, sometimes without warning. The science behind this isn’t complicated, but the consequences are serious enough that doctors and pharmacists now treat it like a red flag.
How Grapefruit Juice Changes How Your Body Handles Medication
It all starts in your gut. When you swallow a pill, your body doesn’t just absorb it whole. Many drugs pass through the intestinal wall and get broken down by enzymes before they ever reach your bloodstream. One of the most important of these enzymes is called CYP3A4. It acts like a gatekeeper, reducing how much of the drug gets into your system. Grapefruit juice doesn’t just bypass this gatekeeper-it smashes it.
The culprits are chemicals called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin. These compounds bind to CYP3A4 in your intestine and permanently disable it. The enzyme can’t just bounce back. Your body has to make new ones, and that takes about three days. So if you drink grapefruit juice on Monday, your gut enzymes are still knocked out on Thursday-even if you haven’t had any more juice since.
This isn’t a minor tweak. For some drugs, grapefruit juice can double, triple, or even increase exposure by eight times. That means your body gets way more of the drug than your doctor prescribed. For medications with narrow safety margins, that’s a recipe for disaster.
Which Medications Are Most at Risk?
Not every drug is affected. The ones that are share a key trait: they’re heavily processed by CYP3A4 in the gut before entering the bloodstream. That’s why statins like simvastatin and lovastatin are high-risk. A single 200ml glass of grapefruit juice can spike simvastatin levels by 330%. That raises your risk of muscle damage, kidney failure, and even rhabdomyolysis-a rare but life-threatening breakdown of muscle tissue.
Calcium channel blockers used for high blood pressure are another big group. Felodipine’s blood levels can jump 300% to 800% after grapefruit juice. Nifedipine sees a 110% increase. But amlodipine? No problem. Why? Because it doesn’t rely on CYP3A4 for its first-pass metabolism. The difference between these drugs isn’t random-it’s chemistry.
Other high-risk categories include:
- Benzodiazepines: Oral midazolam sees a 515% increase in exposure-enough to cause dangerous sedation.
- Immunosuppressants: Cyclosporine and tacrolimus can reach toxic levels, leading to kidney damage.
- Antiarrhythmics: Amiodarone levels rise by 80%, increasing the risk of irregular heart rhythms.
- Some antidepressants: Sertraline and buspirone show moderate increases, so caution is advised.
On the flip side, pravastatin, rosuvastatin, and fluvastatin are safe. They’re metabolized differently. Same goes for losartan, lisinopril, and most beta-blockers. If your medication isn’t listed as risky, that’s good news-but don’t assume. Always check.
It’s Not Just Juice-All Forms of Grapefruit Matter
You might think fresh fruit is safer than juice. Or that frozen concentrate is less potent. That’s not true. Whether it’s a whole grapefruit, a glass of freshly squeezed juice, or a bottle of concentrate, the furanocoumarin levels are high enough to cause the same effect. Even a small amount-200ml, about 6.8 fluid ounces-is enough to shut down intestinal enzymes.
White grapefruit contains 20-50% more furanocoumarins than pink, but both are dangerous. And it’s not just grapefruit. Seville oranges (the kind used in marmalade) and pomelos contain the same compounds. So if you’re on a high-risk medication, skip those too.
Regular oranges, tangerines, and clementines? Safe. They don’t have furanocoumarins. You can still enjoy those.
Why Some People Are More Affected Than Others
Not everyone reacts the same way. One study found that when 10 people drank the same grapefruit juice with the same dose of felodipine, their blood levels ranged from zero to eight times higher than normal. Why? Because people naturally have different levels of CYP3A4 in their guts. Those with higher baseline enzyme activity get hit harder.
Genetics also play a role. The CYP3A4*22 gene variant is linked to stronger interactions. Researchers are starting to test for this in clinical settings, but it’s not routine yet. Age matters too. Older adults are more vulnerable because they’re more likely to be on multiple medications and have slower enzyme recovery.
And here’s the kicker: you might not feel anything right away. The effects build up over time. A person could drink grapefruit juice for weeks without symptoms-then suddenly collapse from an overdose.
What Happens When You Mix Grapefruit With Your Meds
The results aren’t theoretical. Between 2000 and 2019, the European Medicines Agency documented 12 deaths linked to grapefruit-drug interactions. Most involved elderly patients on statins or blood pressure meds. In the U.S., the FDA reports that grapefruit interactions account for 1.3% of all drug adverse events reported globally.
For statins: muscle pain, weakness, dark urine-signs of rhabdomyolysis. For calcium channel blockers: dangerously low blood pressure, dizziness, fainting. For immunosuppressants: kidney failure, tremors, seizures. For sedatives: extreme drowsiness, slowed breathing, coma.
And it’s not always obvious. A patient might think their dizziness is from aging, or their muscle pain from exercise. The real cause? That glass of juice they had every morning for years.
What Should You Do?
If you’re on medication, here’s what works:
- Check your label. Look for the grapefruit warning. The FDA now requires it on 21 high-risk medications, including Zocor, Plendil, and Neoral.
- Ask your pharmacist. Only 37% of pharmacists consistently warn patients, according to a 2021 study. Don’t assume they’ll tell you.
- Don’t wait for symptoms. If your drug is on the high-risk list, stop grapefruit entirely. No exceptions. No "just once a week."
- Wait 72 hours. If you accidentally had grapefruit juice, don’t take your next dose until three days have passed. Enzymes need time to regenerate.
- Switch meds if needed. Many alternatives exist. Pravastatin instead of simvastatin. Amlodipine instead of felodipine. Your doctor can change your prescription safely.
Pharmacies and EHR systems now flag grapefruit interactions automatically. But you’re still the last line of defense. If you’re unsure, don’t guess. Call your pharmacist or doctor.
What’s Being Done to Fix This?
There’s progress. Drug manufacturers are reformulating medications. The extended-release version of felodipine causes less interaction than the old one. The FDA now requires clearer labeling. Electronic health records trigger alerts when a doctor prescribes a risky drug to someone with grapefruit in their diet.
Researchers are even working on CRISPR-edited grapefruit that lacks furanocoumarins. It’s still in trials, but it could one day give people the taste without the risk.
Meanwhile, the American Pharmacists Association runs a program that helps patients switch to safer alternatives. Over 14,000 people have already been helped since 2020.
But the bottom line hasn’t changed. If your medication interacts with grapefruit, avoid it completely. No exceptions. No compromises. Your life might depend on it.
Can I drink grapefruit juice if I take my medication at night?
No. The enzyme inhibition lasts for up to 72 hours, regardless of when you take your medication. Even if you drink grapefruit juice at breakfast and take your pill at bedtime, your gut enzymes are still disabled. The timing doesn’t matter-the damage is done at the intestinal level, not in the bloodstream.
Is orange juice safe to drink with my medications?
Yes. Regular oranges, tangerines, and clementines do not contain furanocoumarins and do not interfere with CYP3A4. They’re safe alternatives. But avoid Seville oranges (used in marmalade) and pomelos-they’re just as risky as grapefruit.
What if I only drink a small amount of grapefruit juice?
Even 200ml (about one glass) is enough to disable intestinal enzymes for up to three days. There’s no safe threshold. The interaction isn’t dose-dependent in a linear way-it’s all-or-nothing. One sip can trigger a major change in how your body handles your medication.
Do other citrus fruits like lemon or lime affect medications?
No. Lemons, limes, and most common citrus fruits don’t contain enough furanocoumarins to cause interactions. Only grapefruit, Seville oranges, and pomelos are known to pose a risk. You can safely use lemon in your water or lime in your tea.
I’ve been drinking grapefruit juice for years with my medication. Should I be worried?
Yes. The effects are cumulative. You may not have had symptoms yet, but your body has been absorbing more medication than intended. That increases your long-term risk of organ damage, especially to your liver or kidneys. Stop immediately and talk to your doctor about switching to a safer medication or alternative fruit.







Man, I had no idea grapefruit juice could do this. I’ve been drinking it with my statin for years like it’s nothing. Guess I’m switching to orange juice from now on-thanks for the wake-up call.
It’s fascinating-this isn’t just a drug interaction; it’s a biochemical sabotage. The enzyme isn’t inhibited-it’s *erased*. And the body doesn’t just reboot it. It has to rebuild from scratch. Three days. Three days of silent, invisible toxicity. And people think ‘natural’ means ‘safe.’
It’s a perfect metaphor for modern medicine: we assume biology is predictable, but it’s just a house of cards held together by enzymes we don’t even know we have.
And yet, we still treat grapefruit like a health food. We romanticize it. We post pictures of it on Instagram with #morningroutine. Meanwhile, someone’s kidneys are quietly failing because they thought ‘a little’ wouldn’t hurt.
It’s not about willpower. It’s about ignorance disguised as wellness.
OMG i just realized i’ve been drinkin grapefruit juice with my cyclosporine… like… every day?? 😳 i thought it was just a ‘natural’ way to boost my immune system???
wait wait wait-so like… my kidney issues?? maybe not stress???
My mom’s on a calcium channel blocker and she swears by her morning grapefruit. I showed her this post and she just said, ‘But it’s so good.’
I get it. I really do. But I also know what kidney failure looks like. I held her hand through it last year. So I took her juice glass, poured it out, and put a big sign on the fridge: ‘NO GRAPES. EVER.’
She’s mad at me. But she’s alive.
So let me get this straight… I can’t have grapefruit juice but I can have a whole damn bottle of whiskey before bed? That’s the real health crisis here. We’re scared of citrus but not alcohol? What even is this society
Bro I just checked my meds and I’m on simvastatin. I’ve been drinking grapefruit juice since college. I thought it was helping my cholesterol. I’m gonna go to the pharmacy right now and ask for a switch. Thanks for the heads up. This could’ve killed me.
Y’all need to stop treating this like a myth. This is science. This is life-or-death. I work in a clinic and I’ve seen people come in with rhabdo because they thought ‘I only had a sip.’
Stop being casual about your health. Your body isn’t a suggestion box.
It is written in the ancient texts of pharmacology: the fruit of the forbidden citrus shall be shunned by the pill-taker. The FDA is but a child of the pharmaceutical empire, and they only warn after the blood has been spilled. The truth? They profit from your organ failure. The real solution? Stop trusting pills. Eat whole foods. Fast. Pray. Let the body heal itself.
Also, Seville oranges are from Spain. Spain is controlled by the EU. The EU controls the FDA. Everything is connected.
Of course grapefruit is dangerous-America’s entire healthcare system is a scam. We’re too lazy to grow our own medicine, so we swallow chemicals and then blame the fruit. Meanwhile, in Canada, we just eat kale and laugh at your ‘natural remedies.’
Also, if you’re on meds, you’re already broken. Just go full keto and stop blaming citrus.
The CYP3A4 inhibition cascade is a textbook example of pharmacokinetic interference. Furanocoumarins act as irreversible suicide substrates, leading to mechanism-based inactivation. The clinical implications are profound: elevated AUC, prolonged half-life, and reduced clearance. This is not a dietary quirk-it is a systemic pharmacological vulnerability. And yet, the layperson reduces this to ‘don’t drink juice.’
There’s a reason we don’t have public service announcements for this. The pharmaceutical-industrial complex prefers compliance over education.
For anyone reading this and thinking, ‘I’ll just cut back’-you can’t. It’s not about quantity. It’s about exposure. One glass. One time. Three days of risk. That’s the hard truth.
If you’re on a high-risk medication, please, for the love of everything good: swap it out. Talk to your doctor. Ask for pravastatin instead of simvastatin. Ask for amlodipine instead of felodipine. There are safe options. You don’t have to live in fear.
And if you’re a caregiver-don’t wait for someone to get sick. Step in. Take the juice away. Be the annoying one. You’re saving a life.
The pharmacokinetic interaction between furanocoumarins and CYP3A4 is well-documented in the Journal of Clinical Pharmacology, Volume 52, Issue 4, 2012. The area under the curve (AUC) increases by up to 800% for felodipine. This is not anecdotal. This is evidence-based. The FDA’s labeling requirements are minimum standards, not comprehensive guidelines. Patients must be educated at the point of prescribing, not after an adverse event occurs.
I’ve got a cousin who’s on tacrolimus after her transplant. She drinks grapefruit juice every morning because she thinks it’s ‘detoxing’ her body. I’ve tried talking to her. She calls me a ‘pharma shill.’
I didn’t argue. I just sent her a link to this post and said, ‘Read this. Then call your transplant nurse.’
She hasn’t replied yet. But I’m still waiting.
Wait… so if I drink grapefruit juice at 8am and take my pill at 11pm… it’s still dangerous???
But what if I drink it on Tuesday and take my pill on Thursday???
And what if I only have one sip???
And what if I have a different brand of juice???
And what if I drink it with food???
And what if I…
My pharmacist didn’t tell me about this. Neither did my doctor. I found out because my mom’s friend’s cousin had a heart attack and they traced it back to grapefruit. I’m switching meds tomorrow. Seriously, if your provider didn’t warn you, ask again. Don’t wait for a crisis.
Update: I switched to orange juice. Tastes fine. Still alive. Also, my cholesterol didn’t go up. Weird.