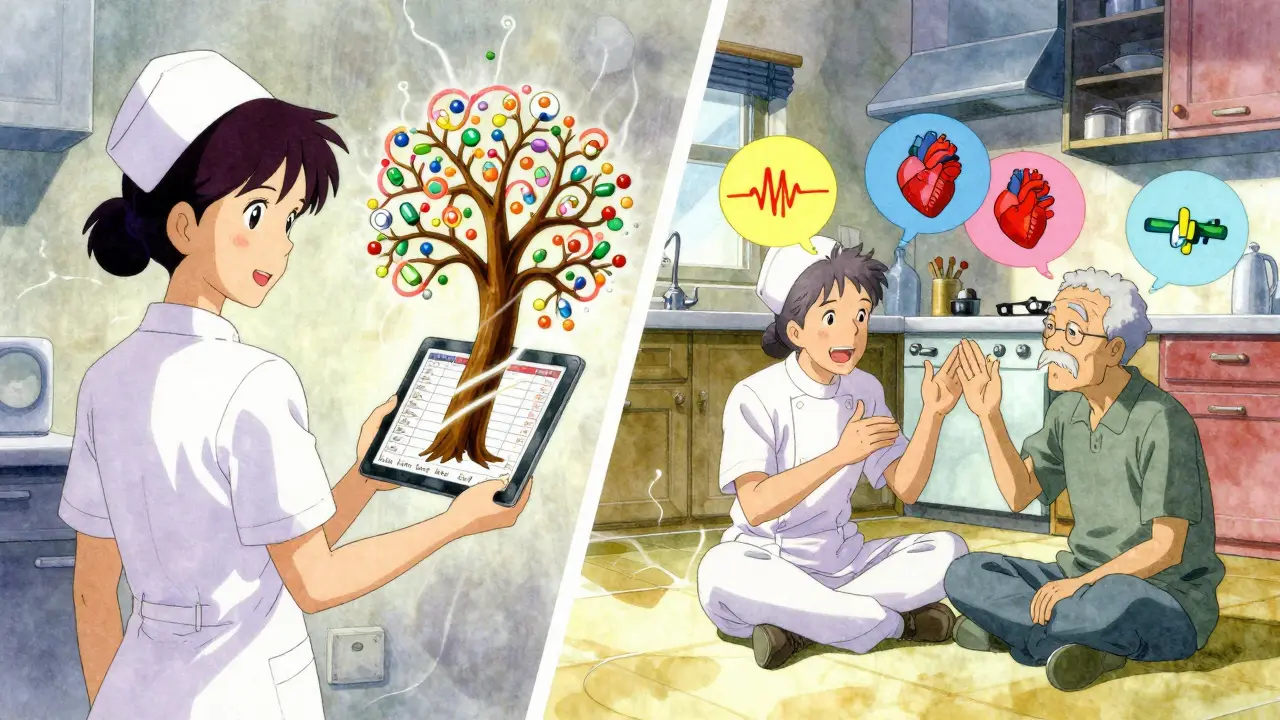
Managing medications at home for an older adult isn’t just about popping pills on time. It’s about avoiding dangerous interactions, remembering which drug does what, and making sure nothing gets missed-especially when someone’s taking five, eight, or even twelve different medicines. That’s where home health services come in. These aren’t just helpers dropping by to remind someone to take their pills. They’re trained professionals who handle the whole system: tracking, organizing, verifying, and documenting every dose to keep seniors safe and out of the hospital.
Why Home Health Services Matter for Medication Management
Every year, about 30% of serious health problems in home care settings come from medication errors. That’s not a small number. It’s not just forgetting a pill-it’s taking the wrong dose, mixing drugs that shouldn’t be together, or missing a critical change in prescription. For seniors on multiple medications, the risk goes up fast. People over 85 are more than twice as likely to need help with meds than those in their early 60s. Home health nurses and aides don’t just hand out pills. They start by making a full list of everything the person is taking-brand names, generics, dosages, why they’re taking it, and any side effects. They check this list against what the doctor ordered. If there’s a duplicate, a dangerous combo, or a drug that’s no longer needed, they flag it. In one case study, Phoenix Home Care’s team caught 12 dangerous medication overlaps in just six months across 200 patients. That’s 12 potential ER visits avoided.What’s Included in a Professional Medication Management Plan
A good home health medication plan has five key parts:- An up-to-date medication list-written in plain language, with both brand and generic names, dosages, times, and the reason for each drug. This list gets shared with every doctor, pharmacist, and caregiver involved.
- A physical organization system-like a pill organizer with compartments for morning, afternoon, evening, and bedtime. Some services use pre-filled daily pouches (like Phoenix Home Care’s WellPack) so the patient just opens one pouch per day.
- Digital reminders-smartphone apps that beep, vibrate, or send texts. Studies show these improve adherence by 35%. Some newer apps even require a fingerprint scan to confirm the pill was taken.
- Teach-back training-the caregiver asks the patient to explain in their own words how and when to take each medicine. If they can’t, the team goes over it again.
- Documentation and reporting-every dose given, missed, or changed is logged in real time. If a dose is skipped, the nurse calls the doctor within hours, not days.
How to Get Started with Home Health Services
The first step is figuring out if you qualify. Medicare Part A covers home health medication management-but only if you meet three rules:- You’re homebound (leaving home takes a lot of effort or medical risk).
- You need skilled nursing care or therapy (not just help with daily tasks).
- A doctor has ordered the services and signed a plan of care.
- The agency sends a nurse to your home for a full medication review. Bring all your pills in a bag-no exceptions. Even supplements and over-the-counter drugs count.
- The nurse compares your list to your prescriptions. They’ll ask: Is this drug still needed? Is the dose too high? Is there a cheaper generic?
- You’ll get a personalized schedule. Maybe your blood pressure pill goes with breakfast, your diabetes med after lunch, and your sleep aid at bedtime.
- You’ll get a pill organizer or daily pouches. The nurse will show you how to use it-and then watch you do it.
- They’ll set up reminders on your phone or give you a simple alarm clock with big buttons.
Real-Life Wins and Common Pitfalls
Mary K. from Ohio started using Phoenix Home Care’s WellPack system after her mom missed nearly a third of her doses. Within two weeks, missed doses dropped to under 5%. She didn’t need to call the pharmacy or check the medicine cabinet every day. Everything was labeled, pre-filled, and easy to open. But it’s not perfect. John T. from Reddit shared how a gap in communication led to a dangerous interaction between blood thinners. His mom was switched to a new drug, but the home health team didn’t get the update from the cardiologist. That’s why coordination matters. Always make sure your home health agency talks directly to your doctor’s office. Another big issue? Timing. One in three caregivers struggle because meds need to be taken at times that clash with daily life-like a pill that must be taken on an empty stomach, but the patient only eats at noon. Good home health teams adjust. They’ll suggest moving a dose to after breakfast if it’s safe. They don’t force the patient to fit the schedule-the schedule fits the patient.Technology Is Changing the Game
In 2023, CritiCare launched a new app that requires a fingerprint scan before a dose can be marked complete. In their pilot group, errors dropped by 40%. Some agencies now include QR codes on pill pouches that link to short videos in 17 languages. That’s huge for non-English speakers. AI tools are coming fast. By 2025, most agencies will use software that scans all your meds and flags possible interactions before they happen. It’s not science fiction-it’s already in use in big cities like Boston and Chicago. But tech alone won’t fix everything. If the person doesn’t understand why they’re taking a pill, they’ll skip it. That’s why the human touch still matters. A nurse who sits down, looks in the patient’s eyes, and says, “This one’s for your heart. If you skip it, you could feel dizzy or worse,” makes a difference no app can match.What Medicare Doesn’t Cover (And How to Fill the Gaps)
Medicare only pays for intermittent visits-maybe two or three times a week. If someone needs daily help, Medicare won’t cover it. That’s where private agencies or family caregivers step in. Some families hire a part-time aide for $15 an hour to hand out pills. But here’s the catch: aides can’t give meds unless they’re trained and supervised by a nurse. Many states require that a nurse visits weekly to check the aide’s work. Another option: ask your pharmacy if they offer medication delivery with daily dosing. Some chains like CVS and Walgreens now offer blister packs with labels for each time of day. It’s not as thorough as a home nurse, but it’s better than nothing.
How to Know If It’s Working
Look for these signs:- Your loved one hasn’t been to the ER or hospital for a medication issue in the last 30 days.
- They can tell you what each pill is for without looking at the bottle.
- The pill organizer is consistently empty at the right times.
- You’re not fielding calls from the pharmacy about missed refills.
- They’re sleeping better, feeling more alert, or have more energy-signs that meds are working as intended.
What to Ask Before Hiring a Provider
Don’t just pick the cheapest option. Ask:- Do you perform medication reconciliation during every visit?
- How do you communicate with my doctor’s office?
- Do you use digital tracking or paper logs?
- Are your staff trained in geriatric meds and the Beers Criteria?
- What happens if a dose is missed?
- Can I see a sample of your medication log?
The Bigger Picture: Why This Matters
Home health medication management isn’t just about avoiding mistakes. It’s about giving seniors back control. When someone knows they’re taking the right pills at the right time, they feel more confident. They sleep better. They don’t fear falling or ending up in the hospital. Studies show patients using these services have 20% fewer hospital readmissions. That’s not just a number-it’s 20% fewer nights in a cold hospital bed, fewer IVs, fewer tests, fewer disruptions to life. And the cost? Clarest’s 2023 study found that for every dollar spent on professional medication management, $5 in hospital costs are saved. That’s a return most insurance companies are starting to notice. This isn’t a luxury. For seniors with complex regimens, it’s a lifeline.Can a home health aide give my parent their medications?
Yes-but only if they’re trained and supervised by a licensed nurse. In most states, aides can hand out pills only under direct nurse oversight. The nurse must review the medication list, confirm dosages, and check for interactions at least weekly. Never let an untrained person manage meds, even if they’re family.
Does Medicare pay for daily medication help at home?
No. Medicare Part A covers only intermittent skilled nursing visits, usually two to three times a week. If daily help is needed, you’ll need to pay out of pocket, use private insurance, or rely on a family member. Some Medicaid programs or VA benefits may cover daily assistance for eligible seniors.
What if my parent refuses to take their meds?
Home health nurses are trained to handle this. They don’t force pills. Instead, they find out why: Is it because of side effects? Confusion? Fear? They’ll work with the doctor to adjust the regimen, switch to a liquid form, or change the timing. Sometimes, just explaining the purpose in simple terms makes all the difference.
How often should the medication list be updated?
Every time there’s a change-new prescription, dose adjustment, or drug discontinued. The home health team should update the list within 24 hours and send the revised version to all providers. Many agencies use digital systems that auto-sync with pharmacy records to reduce delays.
Are there free tools to help manage medications at home?
Yes. The CDC and MedlinePlus offer free printable medication trackers and pill organizers you can download and print. Some pharmacies also offer free blister packs. But these don’t replace professional oversight. For complex regimens, they’re a supplement-not a solution.
What should I do if I suspect a medication error?
Call the home health agency immediately. Then contact the prescribing doctor. Don’t wait to see if symptoms get worse. Keep the pill bottles and any documentation. If there’s a serious reaction, go to the ER and bring the full medication list. Quick action can prevent a life-threatening event.
If you’re caring for someone on multiple medications, you’re not alone. Thousands of families face this every day. The right home health support doesn’t just prevent mistakes-it gives peace of mind. And that’s worth more than any price tag.








Interesting piece. In the UK, we’ve got similar services under the NHS, but access is patchy. I’ve seen elderly neighbors struggle because they’re told ‘it’s not a priority’-even when they’re on 10 meds. The pill organizers help, but nothing replaces a human checking in, really. Just a quick chat can catch a change in cognition or mood before it turns dangerous.
Also, the fingerprint app thing? Brilliant. My gran’s phone is practically a brick, but she loved that it forced her to pause and think before taking anything. No more ‘I already took it’ confusion.
Let’s be real-this whole home health thing is just Big Pharma’s way of keeping seniors hooked on pills. You know they’re making more money off polypharmacy than they ever would from actually curing anything. The ‘medication reconciliation’? That’s just a fancy word for ‘let’s keep prescribing.’
My uncle took 14 pills a day. He got off 11 of them after seeing a functional medicine doc. No nurse needed. Just stopped the nonsense. They call it ‘medication management’-I call it pharmaceutical dependency laundering.
Of course this sounds good on paper. But you’re ignoring the systemic rot underneath. Home health agencies are understaffed, overworked, and underpaid. Nurses are doing 6 visits a day, rushing through med reviews like they’re checking off a grocery list. The ‘digital tracking’? Half the time it’s just a clipboard someone forgot to update.
And don’t get me started on the ‘WellPack’-it’s a branded gimmick. The real issue isn’t the pill organizer-it’s that doctors keep prescribing without ever talking to each other. The system is designed to fail. You fix the paperwork, not the people.
Also, ‘AI flags interactions’? Yeah, right. The AI doesn’t know your grandma’s cat is allergic to aspirin. It doesn’t know she’s been taking ibuprofen for 20 years and her kidneys are shot. You can’t algorithm a human life.
And don’t tell me about ‘20% fewer hospitalizations.’ That’s a statistic pulled from a study funded by the same company that sells the pill pouches. Conflict of interest much?
People don’t need more tech. They need doctors who listen. And if you think a fingerprint scan is safer than a nurse who actually knows the patient’s name, you’re living in a dystopian marketing brochure.
There’s something quietly revolutionary about the teach-back method. It’s not just about compliance-it’s about dignity. When someone can explain why they’re taking a pill in their own words, it means they’re not just a receptacle for pharmaceuticals. They’re an active participant in their care.
I love how the article mentions the 17-language QR videos. That’s not just accessibility-it’s cultural inclusion. My abuela didn’t trust English instructions, but when she watched the video in Spanish showing how the pill looked, she finally felt safe taking it.
And the fact that good teams adjust timing to fit the person’s life? That’s not medical protocol. That’s love in action. Most healthcare systems treat schedules like law. But real care? It bends. It adapts. It whispers, ‘What time works for you?’ instead of ‘You must take this at 8 a.m.’
Also, the $5 return on every $1 spent? That’s not just cost-saving-it’s justice. We spend billions on ER visits because we didn’t invest in the quiet, mundane work of keeping people stable at home. That’s not a service. That’s a moral obligation.
Great breakdown. I’ve worked with home health agencies for years as a caregiver. The key thing people overlook is communication. If the nurse doesn’t talk directly to the prescribing doctor, nothing else matters.
One tip: Always bring the actual bottles-not just a list. Pills get repackaged, labels change, and people forget what the pink one was for. Seeing the bottle, the dosage, the pharmacy stamp-it all clicks.
Also, if you’re using a private agency, ask if they have a pharmacist on staff. Not just a nurse. A pharmacist. They catch way more interactions than nurses can, especially with OTC meds and supplements.
And yes, Medicare’s limits are brutal. But if you qualify, use every visit. Don’t just wait for the med check. Ask for a fall risk assessment, a nutrition review, even a quick cognitive screen. They’re all part of the package.
OMG I just cried reading this. I’ve been the daughter who found my mom with 17 pills in her hand, staring at them like they were alien artifacts. She didn’t know which was which. She was terrified. I thought we were alone.
Then we got Phoenix Home Care. And yes, the WellPack changed everything. But what I didn’t expect? The nurse who sat with her for an hour just listening. Not talking. Not correcting. Just… being there.
That’s the magic no app can replicate. The silence between the pills. The hand on the shoulder. The ‘I see you.’
And now? My mom says she feels like she’s in control again. Not the pills. Not the doctors. HER.
So yes. This isn’t just healthcare. It’s soulcare. And we need more of it.
Medication management is not a technical problem-it is a philosophical one. We have constructed a medical-industrial complex that treats the human body as a machine to be calibrated, rather than a life to be honored. The tools described here-pills organizers, digital trackers, fingerprint scans-are not solutions. They are palliatives.
True healing lies in the relational: in the nurse who remembers the patient’s dog died last year, and asks how the widow is coping. In the aide who notices the tremor in the hand and wonders if it’s the meds or the grief. In the family who sits down at 7 p.m. and says, ‘Let’s open the pouch together.’
Technology amplifies care. But it does not replace it. And when we mistake the former for the latter, we risk turning the most sacred act-caring for the vulnerable-into a transaction.
Let us not celebrate efficiency. Let us celebrate presence.
this is so important i wish more people knew about this like why do we wait till someone ends up in the er why not just help them at home its way cheaper and less scary
bro i had a guy come to my aunt’s house and he just handed her pills like she was a vending machine. no talk no check no nothing. then she had a seizure. turns out the meds were conflicting. home health ain’t always health. sometimes it’s just a paycheck.
they say home health saves money but what they don’t tell you is that the same companies that run these services also own the pharmacies and the pill manufacturers. you think they want you to get better? they want you to keep buying. this whole system is rigged.
why bother with all this when you can just use a pill box from the pharmacy and call it a day