Macrolide Antibiotics QT Prolongation Risk Calculator
Risk Factors Present
When you take an antibiotic for a stubborn chest infection or sinusitis, you expect relief - not a hidden risk to your heart. But for some people, common macrolide antibiotics like azithromycin and clarithromycin can trigger a dangerous heart rhythm problem called QT prolongation, which may lead to a life-threatening arrhythmia known as Torsades de pointes. This isn’t theoretical. It’s documented in thousands of cases, backed by decades of research, and actively shaping how doctors prescribe these drugs today.
What Are Macrolide Antibiotics?
Macrolide antibiotics are a class of drugs that have been used since the 1950s to treat bacterial infections, especially respiratory ones like pneumonia, bronchitis, and strep throat. The most common ones you’ll hear about are azithromycin, clarithromycin, and erythromycin. They work by stopping bacteria from making proteins they need to survive. For many people, they’re safe and effective - which is why azithromycin alone accounts for about 65% of all macrolide prescriptions in the U.S.
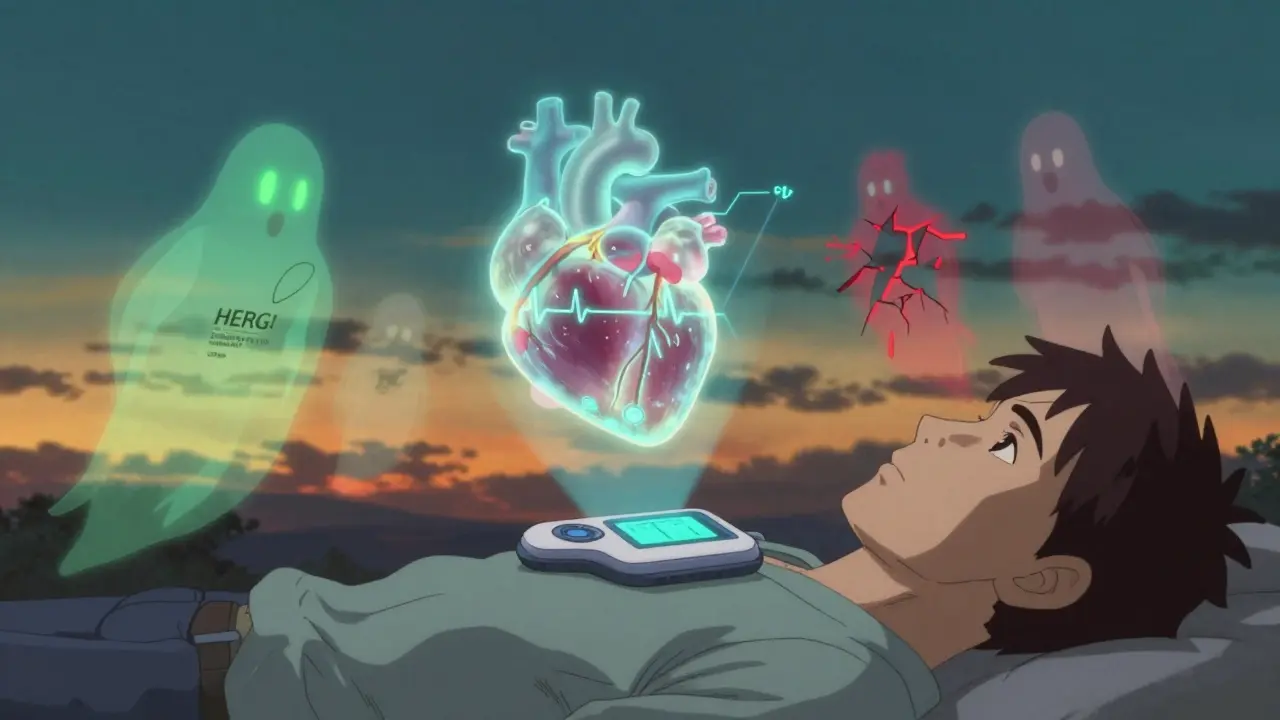
But here’s the catch: these drugs don’t just target bacteria. They also interact with your heart’s electrical system. Specifically, they block a key potassium channel called Ikr, which is encoded by the hERG gene. This channel helps your heart reset between beats. When it’s blocked, your heart takes longer to repolarize - and that delay shows up on an ECG as a longer QT interval.
How QT Prolongation Leads to Arrhythmias
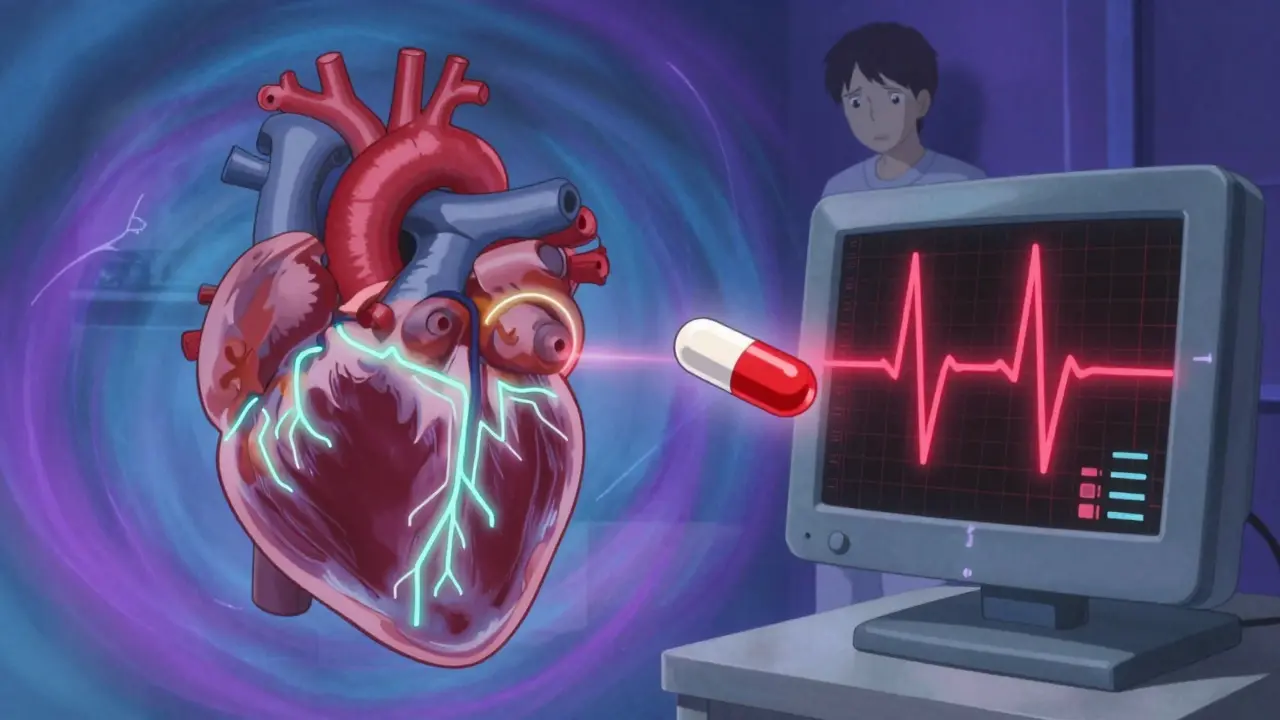
The QT interval on an ECG measures how long it takes your heart’s ventricles to recharge after each beat. A normal QT interval is under 450 ms in men and under 470 ms in women. When it stretches beyond that - especially if it increases by more than 60 ms from your baseline - you’re at risk for Torsades de pointes.
Torsades de pointes isn’t just a weird term. It’s a chaotic, fast heart rhythm that can cause fainting, seizures, or sudden death if not treated immediately. It happens because the prolonged repolarization creates an electrical imbalance between different layers of heart tissue - especially in the mid-myocardial cells. This imbalance sets off abnormal electrical sparks called early afterdepolarizations, which can trigger the dangerous rhythm.
What makes this even trickier is that your QT interval might look normal before you take the antibiotic. But if you have an underlying, undiagnosed genetic condition - like a mild form of long QT syndrome - the drug can push you over the edge. Studies show that 5-20% of people who develop Torsades after taking these antibiotics have no prior history of heart problems. They just had a hidden vulnerability.
Not All Macrolides Are the Same
Here’s where it gets important: not all macrolides carry the same level of risk. Clarithromycin is the most dangerous. It doesn’t just block the Ikr channel - it also strongly inhibits CYP3A4, a liver enzyme that breaks down many other drugs. That means if you’re taking another QT-prolonging medication - say, a statin or an antifungal - clarithromycin can cause those drugs to build up in your blood, multiplying the risk.
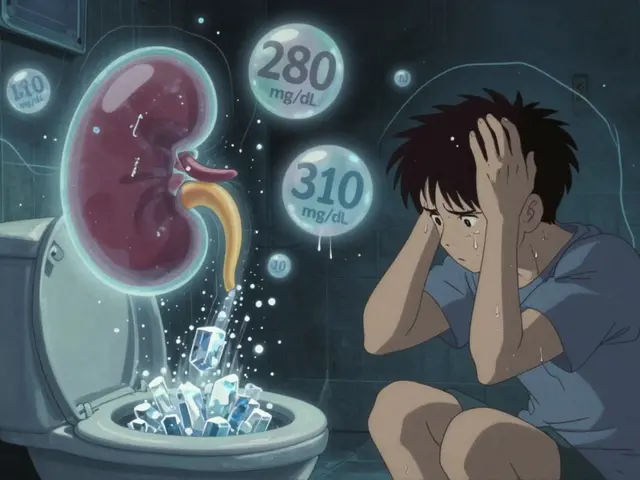
Erythromycin is a bit less potent at blocking Ikr, but it’s notorious for causing severe nausea and vomiting. That can lead to low potassium levels (hypokalemia), which itself prolongs the QT interval. So even if the drug isn’t directly strong, the side effects make it dangerous.
Azithromycin was once thought to be the safest option. It doesn’t interfere much with CYP3A4 and has weaker Ikr blockade. But in 2012, a massive study of 1.3 million people found that azithromycin was linked to a 2.85 excess risk of cardiovascular death per 1,000 courses compared to amoxicillin. That’s not a huge number - but it’s real. And during the early days of the pandemic, when azithromycin was combined with hydroxychloroquine (another QT-prolonging drug), the average QTc increase jumped by 26.2 milliseconds. That’s enough to push many people into dangerous territory.

Who’s at Highest Risk?
If you’re a healthy 30-year-old with no heart issues and no other medications, your risk of Torsades from a macrolide is extremely low - less than 1 in 10,000. But if you have even a few risk factors, that number climbs fast.
Here are the six major risk factors identified in recent guidelines:
- Female sex: Women make up 68% of all documented TdP cases from macrolides.
- Age over 65: Risk doubles compared to younger adults.
- Baseline QTc >450 ms: If your ECG already shows a long QT, your risk jumps nearly fivefold.
- Other QT-prolonging drugs: Taking just one other drug like a diuretic, antidepressant, or antipsychotic increases your risk by 1.8 times per additional drug.
- Low potassium or magnesium: Hypokalemia triples your risk.
- Heart failure or structural heart disease: This raises your risk more than fivefold.
And here’s the part most people miss: you don’t need to have a diagnosed heart condition. A family history of sudden cardiac death before age 50, unexplained fainting, or seizures during exercise could point to an inherited channelopathy. That’s why some cardiologists now ask about family history even if your ECG looks fine.
What Doctors Should Do
Guidelines from the American College of Cardiology and the American Heart Association are clear: don’t just prescribe macrolides blindly. If you have two or more risk factors, get a baseline ECG before starting treatment. If your QTc is over 470 ms in men or 480 ms in women, avoid macrolides entirely.
Also, check your other meds. If you’re on a diuretic, an antidepressant, or a heart rhythm drug, your doctor needs to know. The FDA explicitly says macrolides should be avoided with class IA or III antiarrhythmics - drugs like quinidine or amiodarone - because the combo can be deadly.
For patients already on a macrolide, monitor for symptoms: dizziness, palpitations, fainting, or seizures. If you’re in the hospital or have multiple risk factors, repeat ECGs are recommended. A QTc increase of more than 60 ms from baseline should trigger immediate action - stop the drug and correct electrolytes.
Clarithromycin has a black box warning in the U.S. for QT prolongation. Azithromycin doesn’t - but that doesn’t mean it’s safe. The labeling still includes a warning. The difference in warnings reflects regulatory caution, not safety.
What’s New in Monitoring and Prevention
Technology is catching up. In 2023, the FDA approved a handheld device called the CardioCare QT Monitor that gives accurate QTc readings in under 30 seconds - no lab needed. It’s being used in clinics and urgent care centers to screen patients before prescribing macrolides.
There’s also the Macrolide Arrhythmia Risk Calculator (MARC), developed by Brigham and Women’s Hospital. It uses 12 variables - age, sex, kidney function, current meds, electrolytes, ECG data - to predict your personal risk of TdP with 89% accuracy. It’s not yet in every doctor’s office, but it’s a game-changer for high-risk patients.
Researchers are also working on safer versions of macrolides. Solithromycin showed promise in trials - it blocked Ikr 78% less than clarithromycin - but development was stopped due to liver toxicity. The next frontier? Pharmacogenomics. Early data suggests 15% of people carry genetic variants in the hERG channel that make them far more sensitive to these drugs. In the future, a simple DNA test might tell you if you’re at higher risk before you even take a pill.
Alternatives and When to Avoid Macrolides
If you’re at risk, there are better choices. For respiratory infections, amoxicillin, doxycycline, or levofloxacin (with caution - it also has QT risk) are often preferred. For patients with a history of Torsades or congenital long QT syndrome, macrolides are absolutely contraindicated.
Even if you’re healthy, consider this: most upper respiratory infections are viral. Antibiotics don’t help. If your doctor prescribes azithromycin for a cold, ask why. There’s growing pressure on clinicians to follow antimicrobial stewardship - not just to fight resistance, but to protect hearts, too.
Bottom Line
Macrolide antibiotics are not inherently dangerous. But they’re not harmless either. For most people, the benefits outweigh the risks. But for those with heart conditions, older adults, women, or those on multiple medications, the danger is real - and preventable.
The key is awareness. Know your risk. Know your meds. And if you’re unsure, ask for an ECG. It takes five minutes. It could save your life.
Can azithromycin really cause heart rhythm problems?
Yes. While azithromycin is considered lower risk than clarithromycin or erythromycin, studies show it can still prolong the QT interval and increase the risk of sudden cardiac death, especially in people with existing heart conditions, low potassium, or those taking other QT-prolonging drugs. The risk is small in healthy people but becomes significant with multiple risk factors.
How do I know if I’m at risk for QT prolongation?
You’re at higher risk if you’re female, over 65, have a history of heart failure, low potassium or magnesium, take other QT-prolonging medications, or have a family history of sudden cardiac death. A baseline ECG can show if your QT interval is already long. If you’ve ever fainted during exercise or had unexplained seizures, talk to your doctor about inherited long QT syndrome.
Should I avoid all macrolide antibiotics if I have a heart condition?
Not necessarily - but you need to be cautious. If you have heart failure, a prior arrhythmia, or a QTc over 470 ms, macrolides should generally be avoided. Your doctor can choose safer alternatives like amoxicillin or doxycycline. Never stop or switch antibiotics without medical advice, but do ask about cardiac risks before starting any new drug.
What symptoms should I watch for while taking a macrolide?
Watch for dizziness, lightheadedness, palpitations (feeling your heart race or flutter), fainting, or seizures. These could signal a dangerous heart rhythm. If you experience any of these, stop the medication and seek medical help immediately. Don’t wait to see if it passes - arrhythmias can escalate quickly.
Is there a test to check my risk before taking a macrolide?
Yes. A simple ECG can measure your QT interval. If you have two or more risk factors, a baseline ECG is recommended. In the future, genetic testing for hERG channel variants may help identify those at higher risk, but it’s not yet routine. Tools like the Macrolide Arrhythmia Risk Calculator (MARC) are also emerging and can help estimate your personal risk based on clinical factors.
Can electrolyte imbalances make macrolide risks worse?
Absolutely. Low potassium (hypokalemia) and low magnesium are among the strongest risk factors - they can triple or more your chance of developing Torsades de pointes. Diuretics, vomiting, diarrhea, or poor diet can cause these imbalances. If you’re on a macrolide and taking a water pill, your doctor should check your electrolytes. Don’t assume your levels are fine - get them tested.
Why is clarithromycin riskier than azithromycin?
Clarithromycin blocks the Ikr potassium channel more strongly than azithromycin, and it also inhibits the CYP3A4 liver enzyme, which can cause other QT-prolonging drugs to build up in your blood. This double effect makes it much more likely to trigger dangerous rhythms. Azithromycin has weaker channel blockade and minimal enzyme inhibition, making it safer - but not risk-free.
Are there safer antibiotics for people with heart concerns?
Yes. For most respiratory infections, amoxicillin or doxycycline are preferred over macrolides when cardiac risk is a concern. Levofloxacin is an option too, but it also carries a QT risk, so it’s not always better. The best choice depends on your infection, allergies, and other medications. Always ask your doctor: "Is there a non-macrolide option that’s just as effective?"






So I just took azithromycin for my sinus infection last week and now I’m paranoid every time my heart skips. Like, is this gonna be the day I collapse in Target? 🤡
Hey, I’m a nurse and I’ve seen this firsthand. One elderly patient on clarithromycin + furosemide? QTc shot up to 580ms. She coded in the hallway. We caught it because we checked ECGs routinely. Don’t assume ‘it’s just an antibiotic’ - it’s a cardiac gamble if you’ve got risk factors.
Always ask for a baseline ECG. Five minutes. Could save your life. 💙
As someone raised in the UK where GPs are way more cautious about antibiotics, I’m both relieved and annoyed. Relieved because we’ve been taught to question prescriptions since med school - annoyed because in the US, it feels like antibiotics are handed out like candy at Halloween.
My mum had a near-miss with erythromycin after a bad chest cold. She was on diuretics for hypertension, didn’t know her potassium was low, and ended up in A&E with palpitations. They thought it was anxiety. Turns out, her QT was 510ms. We’ve been careful ever since.
Doctors need to stop treating ‘antibiotics’ like a one-size-fits-all solution. It’s not just resistance we’re fighting - it’s silent cardiac sabotage.
Also, props to that new MARC calculator. If it gets into primary care, we might finally stop treating patients like lab rats.
Let me guess - Big Pharma is hiding this because they make billions off antibiotics. The real danger? The FDA doesn’t ban these drugs because they’re funded by pharma lobbyists. You think they care about your heart? They care about quarterly earnings.
And don’t even get me started on ‘baseline ECGs’ - that’s just another way to make you pay more. My cousin got billed $800 for a 5-minute ECG. Who can afford that?
Meanwhile, the real solution? Stop taking antibiotics unless you’re dying. Which, by the way, most sinus infections aren’t.
Statistical noise. 2.85 excess deaths per 1,000 courses? That’s less than the risk of dying from stepping on a LEGO barefoot.
Meanwhile, the article ignores that macrolides are often the *only* option for penicillin-allergic patients. And yes, QT prolongation is real - but so is sepsis from untreated pneumonia. You’re scaring people into avoiding life-saving drugs over a risk that’s lower than being struck by lightning.
Also, ‘hERG channel variants’? That’s a research curiosity, not a clinical tool. Don’t turn every patient into a genomic experiment.
I’m so glad someone finally said this. I’ve been telling my friends for years: antibiotics aren’t magic pills. My grandma took azithromycin for bronchitis, then passed out in church. Turns out she had undiagnosed long QT. They didn’t even check her meds.
It’s not fear-mongering - it’s just common sense. If you’re on 5 different pills, don’t add another one without asking how it plays with the others.
Also, why is azithromycin still sold like candy? If it can kill, it should need a prescription. And no, ‘over-the-counter’ doesn’t mean ‘safe for everyone’.
Oh wow, so now we’re diagnosing people with ‘hidden channelopathies’ because they took a Z-pack? Next they’ll be screening for ‘subclinical heartbreak’ before prescribing ibuprofen.
Look - if you’re 70, on a water pill, and your ECG looks like a mountain range, sure - get the test. But for the rest of us? Stop treating every cold like a cardiac emergency.
Also, the ‘Macrolide Arrhythmia Risk Calculator’? Cute. Now I need an app to tell me if my coffee will give me atrial fibrillation. 😅
They’re lying. The government knows macrolides cause heart attacks but they won’t admit it because they want you dependent on meds. The real cause of Torsades? 5G radiation + chemtrails messing with your ion channels. They don’t want you to know. The ECG? Just a distraction. The real test is a DNA scan from the moon.
And don’t trust doctors. They’re paid by Big Pharma to ignore the truth.
So let me get this straight - I’m supposed to get an ECG before taking azithromycin for a cold? That’s insane. I’m 32, fit, no meds, no family history. You want me to pay $500 and wait two weeks just to prove I’m not going to die from a sinus infection?
Meanwhile, my cousin died of pneumonia because he didn’t take antibiotics fast enough. You think he’d have waited for an ECG? No. He trusted his doctor. And now he’s gone.
Stop scaring people into avoiding treatment. This isn’t prevention - it’s fear-driven malpractice.
The ethical imperative here transcends mere pharmacological risk-benefit calculus. The normalization of antibiotic prescription without cardiac risk stratification reflects a deeper epistemological failure in contemporary medical practice - a reductionist paradigm that treats the body as a mechanistic aggregate of isolated systems, rather than an integrated bioelectrical organism.
When we prescribe azithromycin as if it were aspirin, we implicitly deny the ontological complexity of cardiac electrophysiology. The hERG channel is not a mere molecular target; it is a sacred conduit of life’s rhythmic integrity.
One cannot ethically dismiss the 2.85 excess deaths per 1,000 courses as ‘statistical noise’ when each number represents a person whose final heartbeat was interrupted not by fate, but by institutional negligence.
True stewardship demands that we elevate precaution to principle - not because every patient is at risk, but because no patient’s life should be treated as expendable in the name of convenience.
Let us not mistake the absence of catastrophe for the presence of safety. The heart does not negotiate with probability.
My mom took clarithromycin and got dizzy. We thought it was the flu. Turns out, she almost died. Never again.
Interesting that the article cites the 2012 JAMA study but doesn’t mention the 2019 meta-analysis in Circulation that showed no significant increase in all-cause mortality when macrolides were used appropriately in low-risk populations. The risk is real, but context-dependent. The real issue? Lack of provider education. We’re not teaching residents how to interpret QT intervals or assess polypharmacy risk. That’s the systemic failure - not the drug itself.
azithromycin is a bioweapon. they put it in the water. they want us weak. the ekg is fake. the hERG channel? a lie. the real cause is the vaccines. they use the same tech. they know what they're doing. i read it on a forum. my cousin's dog got sick after the antibiotic. it's connected.