G6PD Deficiency Risk Assessment
This tool helps you determine if you might be at risk for nitrofurantoin-induced hemolytic anemia due to G6PD deficiency. Based on your responses, it will provide guidance on whether you should discuss G6PD testing with your doctor.
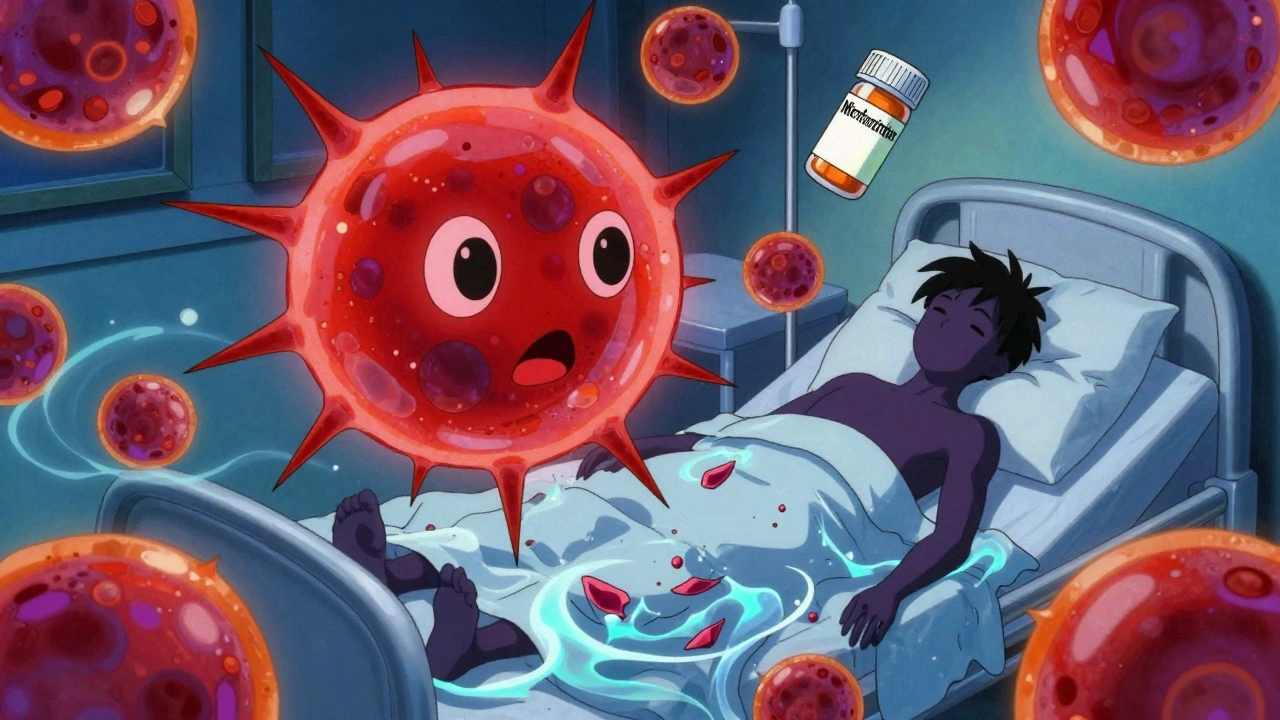
When you get a urinary tract infection, your doctor might prescribe nitrofurantoin. It’s cheap, effective, and often the first choice for simple bladder infections. But here’s something most people don’t know: if you have G6PD deficiency, this common antibiotic can trigger a dangerous drop in red blood cells - a condition called hemolytic anemia. And it can happen fast.
What Is Nitrofurantoin, Really?
Nitrofurantoin, sold under brand names like Macrobid and Furadantin, has been around since the 1940s. It’s not a broad-spectrum antibiotic. It works almost exclusively in the urinary tract. That’s why it’s so popular for uncomplicated UTIs - it concentrates in urine, kills bacteria like E. coli, and doesn’t mess with your gut flora as much as other drugs. About 5.5 million prescriptions are filled for it every year in the U.S. alone.
But here’s the catch: nitrofurantoin doesn’t just attack bacteria. In the body, it creates reactive oxygen molecules. These are great for killing germs, but they’re also toxic to red blood cells - especially if those cells can’t handle oxidative stress.
What Is G6PD Deficiency?
G6PD deficiency is a genetic condition that affects how your red blood cells protect themselves from damage. The enzyme glucose-6-phosphate dehydrogenase (G6PD) helps keep glutathione - your body’s main antioxidant - in working order. Without enough G6PD, your red blood cells can’t fight off oxidative stress. When you take certain drugs, like nitrofurantoin, your red cells start breaking down.
This isn’t rare. Around 400 million people worldwide have it, according to the WHO. It’s most common in people of African, Mediterranean, Middle Eastern, and Southeast Asian descent. In Black populations, up to 14% may be affected. Many people don’t know they have it until they’re exposed to a trigger like nitrofurantoin, fava beans, or certain malaria drugs.
How Nitrofurantoin Triggers Hemolytic Anemia
Within 24 to 72 hours of taking nitrofurantoin, a G6PD-deficient person may start feeling unwell. Symptoms include sudden fatigue, dark urine (like cola or tea), jaundice (yellow skin or eyes), rapid heartbeat, and shortness of breath. Lab tests show falling hemoglobin, rising bilirubin, low haptoglobin, and a spike in reticulocytes - classic signs that red blood cells are being destroyed.
A 2023 case report from the National Center for Biotechnology Information described a patient who developed fever, confusion, vomiting, and low blood pressure after just two days on nitrofurantoin. Their hemoglobin dropped from 13.2 g/dL to 7.1 g/dL in under 72 hours. They were hospitalized but recovered fully after stopping the drug and getting IV fluids. No transfusion was needed.
That’s the pattern. Most cases are reversible if caught early. But not always. A 2022 review of medical literature found 10 deaths linked to nitrofurantoin-induced hemolysis - all in people with undiagnosed G6PD deficiency. Some were pregnant women. Others were infants exposed through breast milk.
Who’s at Risk?
It’s not just about ancestry. If you’re from a region where G6PD deficiency is common - say, your family came from Nigeria, Somalia, Greece, or Cambodia - you’re at higher risk. But even if you don’t know your background, you might still be affected. Studies show 50-60% of people with G6PD deficiency remain undiagnosed until they have a hemolytic crisis.
Pregnant women are especially vulnerable. Nitrofurantoin is often used for UTIs during pregnancy because it’s considered safe for the fetus - unless the mother has G6PD deficiency. In that case, the drug can cross the placenta and trigger hemolysis in the baby. Three documented cases in infants involved maternal exposure.
Older adults with kidney problems are another group at risk. Nitrofurantoin is cleared by the kidneys. If your eGFR is below 60 mL/min, the drug builds up in your blood - increasing toxicity. But many doctors still prescribe it without checking kidney function or G6PD status.
What Do Guidelines Say?
The American Society of Hematology says it plainly: "Avoid nitrofurantoin in patients with known G6PD deficiency." The Clinical Pharmacogenetics Implementation Consortium (CPIC) goes further. They recommend complete avoidance in patients with G6PD deficiency who’ve had chronic hemolytic anemia. For others, they say use with caution - but only if no alternatives exist.
So what are the alternatives? Fosfomycin is a single-dose option that’s safe in G6PD deficiency. Trimethoprim-sulfamethoxazole (TMP-SMX) is common too, but it carries its own risk of hemolysis in G6PD-deficient patients. Fluoroquinolones like ciprofloxacin are effective but come with their own side effects - tendon rupture, nerve damage - and aren’t recommended for first-line use in uncomplicated UTIs.
Why Isn’t Everyone Tested?
Here’s the uncomfortable truth: most doctors don’t screen for G6PD deficiency before prescribing nitrofurantoin. A 2022 survey of 350 primary care physicians found only 32% routinely check G6PD status. Why? Because the FDA label doesn’t require it. The test costs $35-$50. A hospitalization for hemolytic anemia? That’s $8,500 to $12,000.
Some clinics in high-risk areas - like those serving large African or Mediterranean communities - have started routine screening. Electronic health records now sometimes flag high-risk patients. But it’s not standard. Many patients are prescribed nitrofurantoin based on symptoms alone, with no history taken about ancestry, family illness, or previous reactions to drugs.
What Should You Do?
If you’ve ever had unexplained jaundice, dark urine after taking medicine, or a family history of anemia - especially if you’re of African, Mediterranean, or Southeast Asian descent - ask your doctor about G6PD testing before taking nitrofurantoin. It’s a simple blood test. Results come back in hours.
If you’ve been prescribed nitrofurantoin and you’re unsure of your G6PD status, don’t panic. But do monitor for symptoms: fatigue, pale skin, dark urine, yellowing eyes. Stop the drug and call your doctor immediately if any appear.
If you’ve had a reaction before, wear a medical alert bracelet. Tell every provider you see - dentists, ER staff, pharmacists. Nitrofurantoin isn’t the only culprit. Primaquine, sulfonamides, and even some over-the-counter pain relievers can trigger hemolysis in G6PD-deficient people.
The Bigger Picture
Nitrofurantoin isn’t going away. It’s too useful against drug-resistant UTIs. But the way we use it needs to change. The global market for G6PD testing is expected to grow from $185 million in 2022 to $310 million by 2027. Why? Because we’re finally starting to realize that one-size-fits-all prescribing can be deadly.
Research is underway to make point-of-care G6PD tests as easy as a glucose strip. The NIH is running a trial to see if routine testing before nitrofurantoin use saves money and lives. Early data suggests it does.
For now, the safest approach is simple: know your risk. Ask for the test. Push for alternatives if you’re unsure. Your red blood cells can’t defend themselves - but you can.






Nitrofurantoin saved my life last year when I had a UTI that wouldn’t quit - but I had no idea I had G6PD deficiency until I turned yellow and felt like I’d been hit by a truck. Turns out my dad had it too. They didn’t test me. No one ever does. If you’re from a Black, Mediterranean, or Southeast Asian background - get tested before you take it. Seriously. It’s a $35 blood test. Not worth risking your kidneys or your life for a cheap antibiotic.
Wear a medical alert bracelet. Tell every doctor. Even the dentist. I did. Now I’m fine. But I almost didn’t make it.
There’s a systemic failure here. Medicine still operates on the assumption that ‘normal’ means white, male, and genetically homogeneous. G6PD deficiency isn’t some rare oddity - it’s one of the most common enzymopathies on the planet. And yet we’re still prescribing nitrofurantoin like it’s water. The fact that the FDA doesn’t mandate screening is a scandal. It’s cheaper to test than to hospitalize. We’re not just being negligent - we’re profiting off ignorance.
This isn’t about individual risk. It’s about institutional arrogance.
lol so basically if you’re black or mediterranean you can’t take antibiotics? what’s next, no aspirin for people with red hair? this is just medical racism dressed up as science. everyone gets sick, why should one group get special treatment? just don’t take the drug if you’re scared.
also why is everyone acting like this is new? i’ve known about this since high school bio.
From a clinical pharmacogenomics standpoint, the CPIC guidelines are unequivocal: nitrofurantoin is contraindicated in G6PD-deficient individuals due to NADPH depletion leading to unchecked oxidative stress in erythrocytes. The enzyme’s polymorphic variants - particularly the Mediterranean and A- alleles - confer heightened susceptibility to hemolysis via reactive oxygen species accumulation.
Point-of-care diagnostics are advancing rapidly; the WHO-endorsed fluorescent spot test has >95% sensitivity. Yet, in primary care settings, 68% of providers still fail to integrate pharmacogenetic risk stratification into UTI management protocols. This represents a critical gap between evidence and practice.
It’s not that complicated. If you’re from a population with known G6PD prevalence and you’re being prescribed a drug with a known hemolytic risk, you’re either lazy or incompetent if you don’t test first. The fact that this is even a debate is embarrassing. We’re not talking about theoretical risk - we’re talking about people dying in ERs because a doctor didn’t ask two questions.
And yes, I’m calling out the entire medical establishment. You’re not protecting patients. You’re protecting billing codes.
okay but like… i just got prescribed this and i’m not even sure what g6pd is and now i’m paranoid and also my urine looks kinda brown?? is this a thing?? should i stop??
also can i just take a vitamin instead??
Wesley - stop panicking. But also - stop taking it. Call your pharmacy right now. Ask if they have a copy of your G6PD status on file. If not, go to urgent care and get a finger-stick test. It takes five minutes. You don’t need a doctor’s order in most states.
And if you’re pregnant or have kids - this isn’t just about you. Nitrofurantoin crosses the placenta. It’s in breast milk. You’re not just risking yourself. You’re risking a baby. That’s not fearmongering. That’s biology.
thank you for this post. i’m black and i had no idea i had this. i took nitrofurantoin last year and got super tired and my eyes turned yellow but i thought it was just the flu. now i know. i got tested and i’m positive. i’m telling my mom and my sister. we’re all getting checked. this could’ve killed us.
please share this. someone’s life could depend on it.