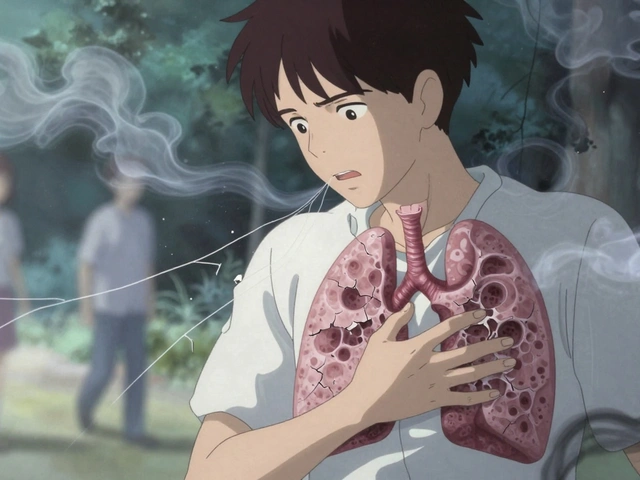
When pain becomes a daily companion-whether it's a nagging lower back ache, stiff knees from arthritis, or tight shoulders from sitting at a desk all day-most people reach for pills first. But what if the real solution isn't in a bottle, but in movement? Physical therapy for pain isn't just about easing discomfort. It's about restoring how your body works, one controlled motion at a time.
Why Movement Heals More Than Medication
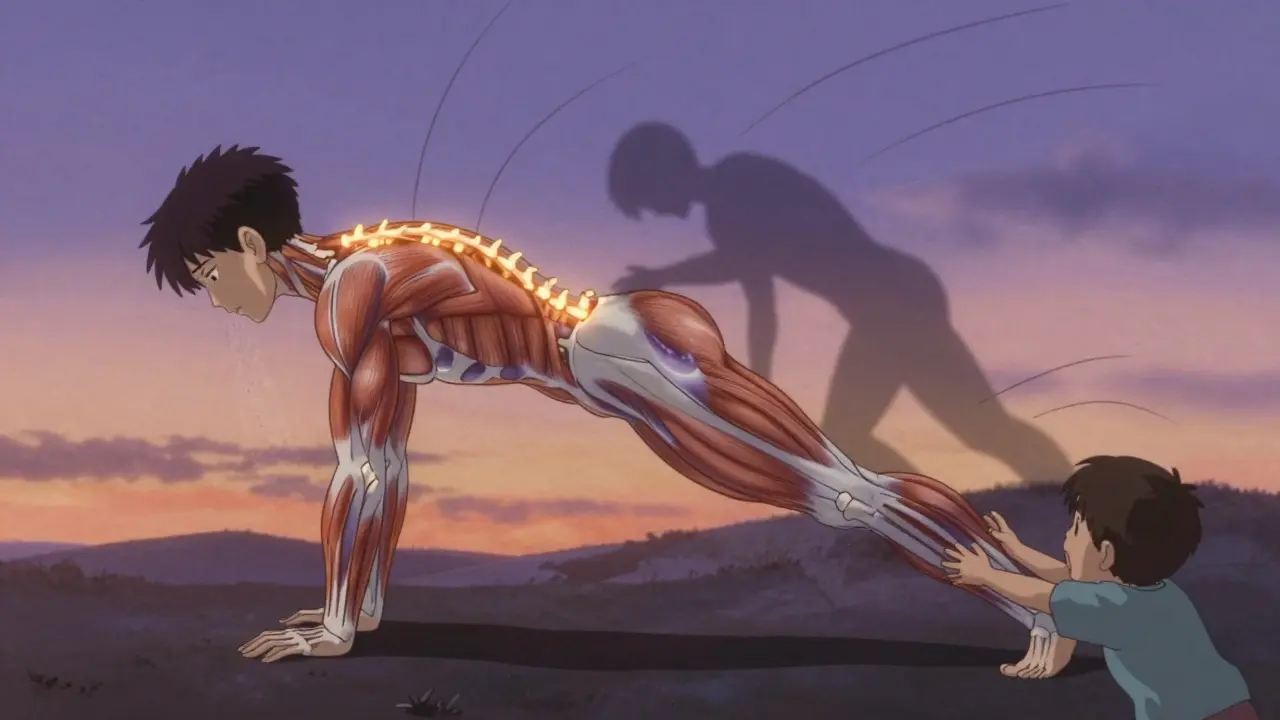
Pain isn't always a sign of damage. Often, it's a signal that something's out of balance. Muscles weaken. Joints stiffen. Nerves get hypersensitive. Medications can mask the pain, but they don't fix the cause. Physical therapy does. Studies show that structured exercise and stretching can reduce pain by 50-75% in just 6 to 8 weeks. That’s not luck. It’s science.The body responds to movement by releasing natural painkillers-endorphins. It also calms overactive nerves. When you move correctly, you teach your nervous system that motion is safe. That’s the core of pain restoration: rewiring your brain’s response to movement so it stops sounding the alarm when it doesn’t need to.
Exercise That Actually Works for Pain
Not all exercise is created equal when you’re in pain. High-intensity workouts can make things worse. The key is finding the right dose.For most types of chronic pain-back pain, osteoarthritis, fibromyalgia-the sweet spot is moderate aerobic activity: walking, swimming, or cycling at 65-75% of your maximum heart rate. That’s not sprinting. That’s a pace where you can talk but not sing. Do it for 20-30 minutes, three to five times a week. A 2023 Mayo Clinic study found water-based exercises cut knee joint stress by 50% compared to walking on land, making swimming ideal for joint pain sufferers.
Strength training matters too. Two to three sets of 8-15 reps at 60-80% of your one-rep max, targeting major muscle groups like glutes, core, and back, helps stabilize joints and take pressure off painful areas. Progress slowly-add 5-10% more resistance each week. No need to lift heavy. Just lift consistently.
And here’s something surprising: short bursts work. A Duke University study with office workers showed that just two minutes of targeted exercises daily reduced neck and shoulder pain nearly as much as 12-minute sessions. That’s the power of micro-movements. You don’t need hours. You need consistency.
Stretching: Not Just for Yoga Fans
Stretching isn’t about touching your toes. It’s about regaining freedom of movement. When muscles tighten from inactivity or injury, they pull on joints, creating pain. Static stretching-holding a stretch without bouncing-for 30 to 60 seconds, five to seven days a week, can increase range of motion by 15-25 degrees in just four weeks.Focus on the areas that matter most:
- Lower back: Knee-to-chest stretches, cat-cow movements
- Neck and shoulders: Gentle chin tucks, ear-to-shoulder stretches
- Hips and hamstrings: Seated forward bends, reclined leg stretches
And don’t forget breathing. Many people hold their breath when stretching, which tenses muscles instead of relaxing them. Inhale deeply through your nose, exhale slowly through your mouth as you ease into the stretch. It doubles the effect.

Restoration: Getting Back to Life
Pain doesn’t just hurt. It limits. You stop walking far. You avoid stairs. You skip playing with your kids. Restoration means rebuilding those habits-safely.Physical therapists use a method called graded activity. You start small. Maybe you walk five minutes instead of ten. You increase by 10-15% each week. The rule? If pain stays below 3 out of 10 during exercise and returns to normal within an hour after, you’re on track. If it spikes higher or lingers past two hours, you’ve pushed too hard. Adjust. Try again tomorrow.
One of the most powerful tools is the two-hour pain rule. If pain flares up after exercise but fades within two hours, it’s a normal response-not a warning sign. Many people quit because they mistake this for failure. It’s not. It’s part of the process.
What Works Best for Specific Pain Types
Different pains need different approaches.Osteoarthritis: Low-impact cardio like swimming or cycling reduces pain by 35-40%. Strength training for quads and hamstrings supports the knee joint. A 2023 study showed water exercise was twice as effective as land walking.
Fibromyalgia: Tai chi outperforms standard aerobic exercise. A 2022 Arthritis Foundation trial with nearly 300 people found tai chi reduced pain 30% more than walking or biking. Why? It combines movement, breath, and mindfulness-calming the nervous system while gently activating muscles.
Chronic back pain: Targeted core and glute exercises are key. Dr. James Fricton from UT Health Austin reports 70% success in reducing chronic back pain with properly done home programs. Exercises like bird-dogs, bridges, and dead bugs strengthen the muscles that support your spine without jarring it.
Neck and shoulder pain: Office workers see 31% pain reduction after four weeks of two-minute routines using resistance bands. Simple movements like shoulder blade squeezes and chin tucks make a big difference.
Common Mistakes and How to Avoid Them
Many people try physical therapy and give up because they feel worse at first. That’s usually not the therapy’s fault-it’s the approach.Mistake 1: Going too hard too fast. Pushing into sharp pain triggers inflammation and fear. Pain should never spike above 3-4/10 during exercise. If it does, back off.
Mistake 2: Skipping form for speed. Doing 20 leg raises with poor technique won’t help. One perfect repetition is better than ten sloppy ones. Watch videos. Ask a therapist. Record yourself.
Mistake 3: Thinking it’s a quick fix. Physical therapy isn’t a one-time visit. It’s a lifestyle shift. Adherence rates jump from 45% to 78% when patients get video demos of their exercises. Keep them on your phone. Do them like brushing your teeth.
Mistake 4: Ignoring breathing and posture. Slouching while stretching or holding your breath during lifts defeats the purpose. Good posture and slow breathing are silent superpowers.
What to Expect from a Physical Therapist
Not all physical therapy is the same. In academic medical centers, sessions last 45 minutes with one-on-one attention. In corporate clinics, you might get 30 minutes with the therapist juggling two or three patients.Ask for:
- A clear written or video plan of your exercises
- Explanation of why each movement matters
- Pain monitoring guidance (what’s normal, what’s not)
- Progression plan (how to increase over time)
If you’re handed a handout with no explanation, or told to just “do these,” find someone else. Good therapy is personalized, not generic.
The Bigger Picture: Why Physical Therapy Is the Future
The global non-opioid pain market hit $58.3 billion in 2023. Physical therapy makes up over 20% of that-and it’s growing fast. Why? Because people are tired of pills with side effects. Because insurers are pushing for cheaper, safer options. Because Medicare now covers 80% of approved physical therapy visits.The American College of Physicians now recommends physical therapy as a first-line treatment for back pain-before medication. That’s a huge shift. And it’s not just for older adults. Adults 45-64 make up 38% of patients, but younger people are catching on. More clinics now offer telehealth sessions and wearable sensors to track movement and form at home.
Even the Arthritis Foundation updated its two-minute exercise protocol in January 2024, expanding it to 12 joint conditions. The NIH funded $14.7 million in 2023 to study ultra-short exercise routines for chronic pain. The message is clear: movement is medicine. And it’s getting smarter.
You don’t need to be fit to start. You just need to move. One stretch. One walk. One set of exercises. Day after day. Pain doesn’t vanish overnight. But with the right movement, it fades. And so does the fear. And then-you get your life back.
Can physical therapy help with chronic pain without medication?
Yes. Multiple studies show that structured exercise and stretching reduce chronic pain by 50-75% in 6-8 weeks. Physical therapy works by strengthening muscles, improving joint movement, and calming overactive pain signals in the nervous system. It’s not a quick fix, but it addresses the root cause, not just the symptom.
How long should I stretch for pain relief?
Hold each stretch for 30 to 60 seconds, repeating 2-3 times per muscle group. Do this 5-7 days a week. Studies show this duration increases range of motion by 15-25 degrees in four weeks. Don’t bounce. Breathe slowly. Focus on relaxation, not pushing into pain.
Is walking enough for back pain?
Walking helps, but it’s not enough on its own. For lasting relief, combine walking with core-strengthening exercises like bridges, bird-dogs, and planks. These stabilize your spine and take pressure off painful areas. A 2023 Mayo Clinic protocol showed 62% pain reduction in six weeks when walking was paired with targeted strength work.
Why does exercise sometimes make my pain worse?
It’s often because you’re moving too fast or with poor form. Pain during exercise should stay below 3/10 and fade within an hour. If it spikes higher or lasts more than two hours, you’ve pushed too hard. Back off, slow down, and check your technique. Mild soreness is normal; sharp or lingering pain is not.
Do I need a physical therapist, or can I do this at home?
You can start at home with proven protocols like the Arthritis Foundation’s two-minute routines or Mayo Clinic’s back exercises. But if pain persists, or you’re unsure about form, seeing a therapist for 2-3 sessions is worth it. They’ll tailor the plan to your body, correct mistakes, and prevent injury. Home programs work best when they’re personalized and backed by expert guidance.
How soon will I feel better with physical therapy?
Some people feel less pain after just a few days of consistent movement. But meaningful, lasting improvement usually takes 4-6 weeks. The key is consistency-not intensity. Doing 10 minutes a day, five days a week, will beat a 60-minute workout once a week. Progress is slow, but steady.
Is tai chi better than regular exercise for fibromyalgia?
Yes. A 2022 Arthritis Foundation trial found tai chi reduced fibromyalgia pain 30% more than standard aerobic exercise over 12 weeks. Its combination of slow movement, breath control, and mindfulness helps calm the nervous system, which is often overactive in fibromyalgia. You don’t need to be flexible-just willing to move gently.
What’s the best way to stay consistent with physical therapy exercises?
Link your exercises to a daily habit-like brushing your teeth or having morning coffee. Use video reminders on your phone. Track progress in a simple journal. Studies show adherence jumps from 45% to 78% when patients have visual guides. Don’t rely on memory. Make it easy. Make it routine.





Man, this is the kind of post that makes me want to get up and move right now. I used to pop ibuprofen like candy until I tried physical therapy for my lower back. Started with 10 minutes of walking and a few cat-cows. Four weeks later? I played basketball with my nephew without wincing. It’s not magic-it’s just consistent, smart movement. Stop waiting for a pill to fix what your body’s begging you to fix with motion.
Correct form matters more than duration. One perfect bird-dog is worth ten sloppy ones. Focus on control, not speed. And breathe. Always breathe.
They don't want you to know this, but physical therapy is just a front for the pharmaceutical industry to sell you more meds later. They get you hooked on ‘movement’ so you’ll keep coming back for ‘progressive’ treatments. You think your back pain is from sitting? It’s from EMFs and fluoride in the water. Move all you want-it won’t fix what they’ve poisoned you with.
I’ve been doing this for 11 months now, and I’ve seen changes I didn’t think were possible. I used to cry just getting out of bed. Now I walk 2 miles every morning before work. It’s not easy. Some days I want to quit. But I stick to the two-hour rule-pain flares, but it fades. I track everything in a notebook. I even started doing the two-minute shoulder squeezes while waiting for my coffee. It’s not glamorous. But it’s mine. I’m not just surviving anymore. I’m living. And I didn’t need a single prescription to do it. No one told me this would work. But it did. And now I’m telling you. Don’t give up. Just move. Even if it’s slow. Even if it’s small. Even if it’s just one stretch. One day. One breath. One step.
There’s something deeply spiritual about moving through pain instead of numbing it. We’ve been taught to fear discomfort, but what if pain is just our body whispering, ‘Hey, you forgot how to be alive’? Stretching isn’t about flexibility-it’s about relearning trust. Trust in your body. Trust in time. Trust that healing isn’t a race. It’s a rhythm. And sometimes, the most radical act is simply showing up for yourself, one breath, one movement, one quiet morning at a time.
Just did the two-minute neck routine before my Zoom call. Felt like a whole chiropractor visit in 90 seconds. 🤘 Seriously, if you sit at a desk, do chin tucks every hour. Your future self will high-five you. Also-swimming saved my knees. Water is basically magic. Try it. You won’t regret it.
While the anecdotal evidence is compelling, one must interrogate the methodological rigor of the cited studies. The Mayo Clinic water exercise data, for instance, lacks adequate control for confounding variables such as hydration status and thermal regulation. Moreover, the self-reported pain metrics are inherently subjective and vulnerable to placebo effects. Until longitudinal, double-blind RCTs are published with validated outcome measures-such as the Oswestry Disability Index or VAS with inter-rater reliability-this remains pseudoscientific populism masquerading as evidence-based practice.
Wait, so if tai chi works better than walking for fibromyalgia, is it because of the breathwork, the mindfulness, or just the fact that it’s low-impact? Or is it the community aspect? I’ve seen studies where group movement beats solo exercise. Maybe it’s not the movement-it’s the belonging. Should we be prescribing social connection along with stretches? Just wondering.
Can you send me the exact link to the NIH-funded study on ultra-short routines? I want to check the funding source and see if there’s any conflict of interest with physical therapy associations. Also, how many participants were in the Duke office worker study? I need to know the sample size before I trust it.
They’re pushing this ‘movement is medicine’ crap because the government wants to cut Medicare costs. They don’t care if you get better-they care if you stop taking opioids. And don’t even get me started on how they’re using telehealth to replace real PT. They’re just trying to get you to do it yourself so they don’t have to pay for a real therapist. This is all a cover-up. I saw a video of a guy doing bird-dogs on YouTube and now he’s got a herniated disc. They don’t warn you about that.
Why do people think stretching is ‘yoga for hippies’? I stretch every morning-knees to chest, ear-to-shoulder, seated forward bend-and I haven’t taken a pain pill in 18 months. It’s not complicated. It’s not spiritual. It’s just physics. Tight muscles pull bones out of alignment. Loosen them. Stop overthinking it. Do the stretches. You’ll feel better. End of story.
^^^ This. I used to think I needed a fancy gym or a trainer. Nah. Just do the cat-cow while you wait for your coffee. Do the chin tucks while you’re on hold with customer service. Movement doesn’t need permission. It just needs you.