When your skin breaks out in scaly patches and your fingers swell like sausages, it’s not just bad luck - it’s your immune system attacking itself. Psoriatic arthritis isn’t two separate problems. It’s one disease with two faces: one on your skin, the other in your joints. And if you’ve got psoriasis and now your knuckles ache or your toes feel stiff in the morning, you’re not imagining it. This is psoriatic arthritis, and it’s more common than you think.
How Skin and Joints Are Connected
Psoriatic arthritis doesn’t appear out of nowhere. It shows up in about 30% of people who already have psoriasis. But here’s the twist: for 15% of people, joint pain comes first. You might limp for months before you notice that red, flaky patch behind your ear or on your scalp. That’s why doctors say: if you have psoriasis, watch your joints. And if you have unexplained joint pain, check your skin - even if it looks fine.
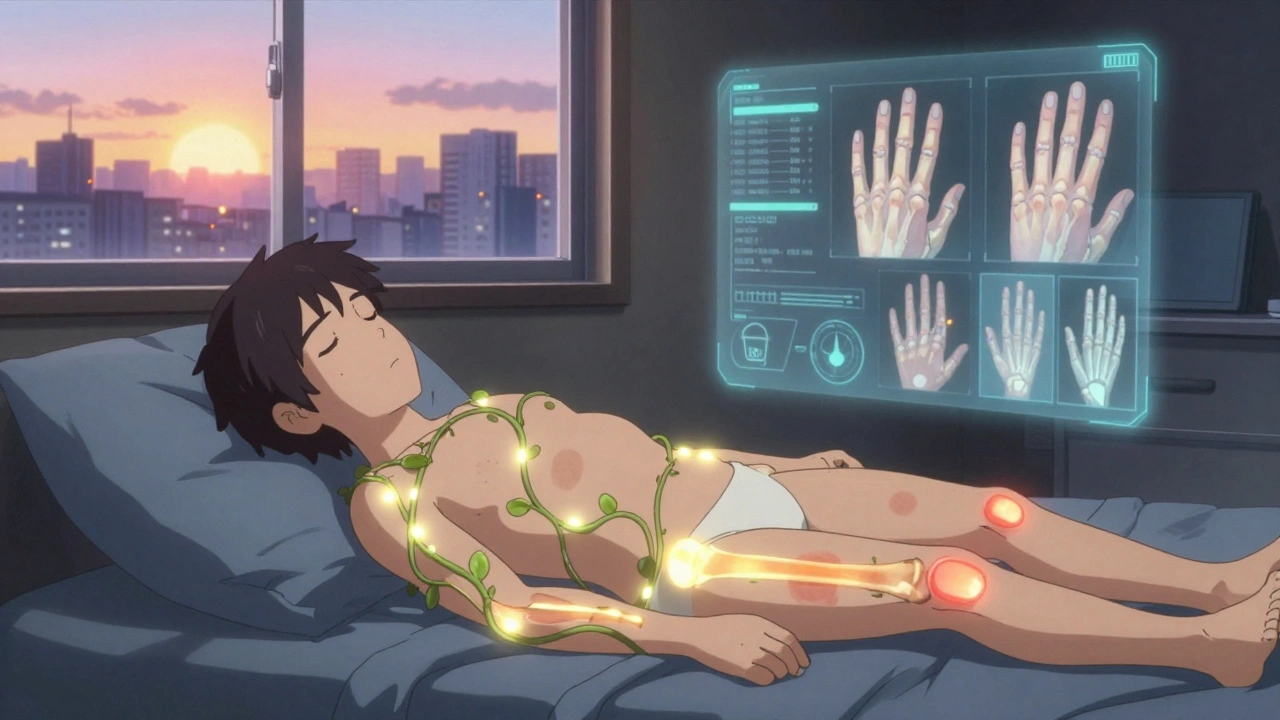
The same immune cells that flare up on your elbows and knees also invade the lining of your joints and the places where tendons attach to bone. That’s why you get both plaques and pain. It’s not coincidence. It’s biology. The inflammation doesn’t stop at the surface. It digs deep.
Signs You Can’t Ignore
Not all joint pain is the same. If you’ve been told you have “just arthritis,” but your symptoms don’t match what you’ve read about rheumatoid arthritis, pay attention. Psoriatic arthritis has unique fingerprints.
- Dactylitis: One or more fingers or toes puff up like sausages. No swelling in the middle - the whole digit swells. This happens in 40-50% of cases and is rare in other types of arthritis.
- Enthesitis: Pain where tendons meet bone. Think bottom of your heel (plantar fasciitis), back of your ankle (Achilles tendon), or even where your rib cage meets your breastbone. It’s not muscle strain. It’s inflammation at the attachment point.
- Nail changes: Pitting, ridges, or your nail lifting off the nail bed (onycholysis). Eight out of ten people with psoriatic arthritis have these. If you’ve got nail problems and joint pain, it’s a red flag.
- Asymmetric joint pain: Your right knee hurts, but your left knee is fine. Your left wrist swells, but your right one doesn’t. Unlike rheumatoid arthritis, which usually hits both sides equally, psoriatic arthritis plays favorites.
- Distal joint involvement: The joints closest to your fingernails and toenails are often the first to go. That’s unusual. Most arthritides start in the knuckles or wrists.
And don’t forget the skin. Plaque psoriasis - thick, red patches with silvery scales - is the most common. But some people get inverse psoriasis in skin folds, guttate psoriasis after a sore throat, or even pustules on their palms. The skin and joints don’t always flare together, but they’re linked.
Why Diagnosis Takes So Long
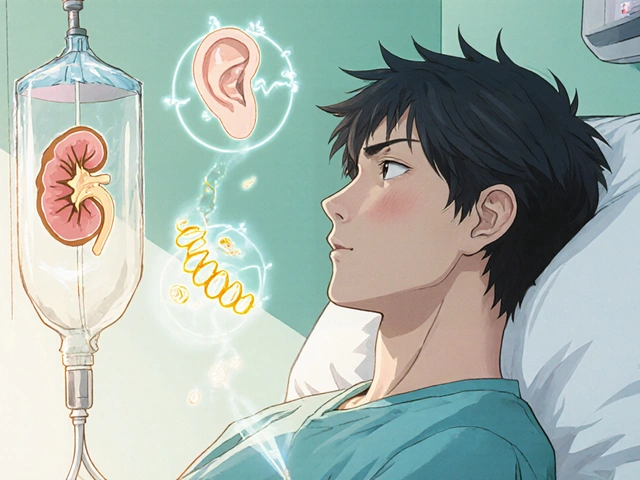
On average, people wait 2.3 years to get the right diagnosis. Why? Because there’s no blood test for it. No single marker like rheumatoid factor. Your blood might look normal, even while your joints are being eaten from the inside.
Doctors rely on patterns: skin lesions + joint pain + nail changes + asymmetry. X-rays and MRIs help show bone erosion or enthesitis, but they’re not always clear early on. Many patients are misdiagnosed with rheumatoid arthritis or osteoarthritis. One Reddit user, ‘PsOwarrior87,’ spent five years on the wrong meds before switching to ustekinumab. That’s five years of unnecessary pain.
That’s why dermatologists play a key role. Nearly half of psoriatic arthritis cases are first spotted by skin specialists - not rheumatologists. If your dermatologist says, “Check your joints,” don’t brush it off.

Treatment That Actually Works
There’s no cure. But there’s control. And it’s better than ever.
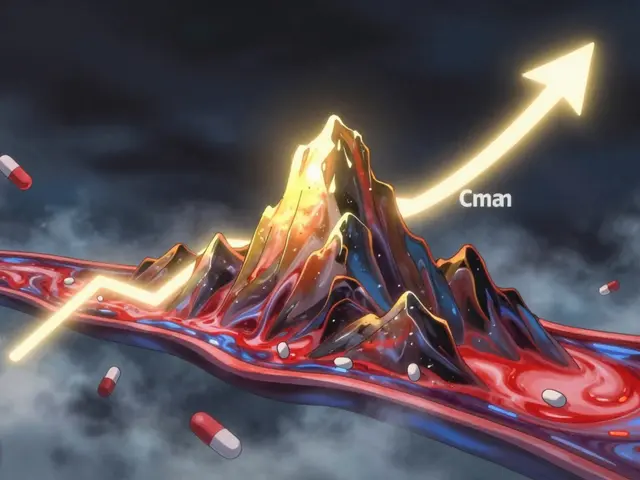
Twenty years ago, treatment meant methotrexate and hoping for the best. Now, we have biologics - drugs that block specific parts of the immune system driving the inflammation. These aren’t just painkillers. They stop the damage.
- TNF inhibitors: Like adalimumab (Humira) and etanercept (Enbrel). They’ve been around since the early 2000s and still make up over half of biologic prescriptions.
- IL-17 and IL-23 blockers: Guselkumab (Tremfya), secukinumab (Cosentyx), and others target different parts of the immune chain. Many patients report dramatic improvements - one user went from two hours of morning stiffness to 20 minutes in six weeks.
- TYK2 inhibitors: Deucravacitinib (Sotyktu), approved in 2022, is the first oral drug in this class. No injections. Just a pill. And it works for both skin and joints.
- DMARDs: Methotrexate and sulfasalazine are still used, especially early on or in milder cases. They’re cheaper but slower and less effective for severe disease.
Studies show that if you start treatment within 12 weeks of symptoms, you can prevent irreversible joint damage in 75% of cases. Delay treatment, and 30% of people will have serious joint destruction within two years.
What Doesn’t Work (and Why)
Not every treatment works for everyone. And some side effects surprise people.
Biologics can trigger new skin flares. Ustekinumab helped one person’s joints - but gave them a bad scalp psoriasis outbreak. Another might get a rash, infection, or fatigue. The immune system is a complex machine. Shutting down one part can cause another to misfire.
And cost? That’s a real barrier. Nearly 80% of patients pay more than $500 a month out of pocket for biologics. Insurance approvals take an average of 14.7 business days. Some people skip doses or delay starting because of the price.
Even when joints feel better, “brain fog” lingers for over half of patients. It’s not just tiredness. It’s mental cloudiness, memory lapses, trouble focusing. We still don’t fully understand why - but it’s real.
How to Take Control
Managing psoriatic arthritis isn’t just about pills. It’s a team sport.
- See both a rheumatologist and dermatologist. Coordinated care improves outcomes by 85%. One specialist can’t see the whole picture.
- Learn your triggers. Stress, infections, alcohol, and certain foods can spark flares. It takes 3-6 months to spot your personal patterns.
- Move your body. Gentle exercise - swimming, yoga, walking - keeps joints flexible and reduces stiffness. Physical therapy isn’t optional. It’s essential.
- Test for TB and hepatitis. Before starting biologics, you need these screenings. It’s not a formality - it’s life-saving.
- Track your symptoms. Use a journal or app. Note joint pain levels, skin changes, sleep quality, and fatigue. That data helps your doctor adjust your treatment faster.
And don’t wait for a crisis. The goal isn’t just to feel better. It’s to reach “minimal disease activity.” That means almost no swelling, no new damage, and no major flares. It’s achievable - for 40-60% of patients on combination therapy.
What’s Next?
The future is getting brighter. AI tools can now predict who with psoriasis will develop arthritis with 87% accuracy - just by analyzing photos of nails and joints. That means earlier intervention.
New oral drugs like upadacitinib (a JAK inhibitor) are in late-stage trials. If approved, they’ll give people more options than injections. By 2028, genetic testing could tell you which drug will work best for you - cutting out years of trial and error.
And while heart disease risk is still 1.5 times higher for people with psoriatic arthritis, studies show that with proper treatment, life expectancy is nearly normal. The disease doesn’t have to define you.
Can you have psoriatic arthritis without psoriasis?
Yes, but it’s rare. About 15% of people develop joint symptoms before any visible skin changes. Still, most will develop psoriasis within a few years. If you have unexplained joint pain, especially with nail changes or family history of psoriasis, get checked - even if your skin looks fine.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis usually affects joints symmetrically - both hands, both knees. Psoriatic arthritis is often asymmetric. It also causes dactylitis, enthesitis, and nail changes, which are rare in rheumatoid arthritis. Blood tests for rheumatoid factor are negative in 90% of psoriatic arthritis cases, making diagnosis trickier.
Do biologics cure psoriatic arthritis?
No cure exists yet. But biologics can stop joint damage, reduce pain, and push the disease into long-term remission. Many people live with minimal symptoms for years. Stopping treatment often leads to flare-ups, so most need ongoing therapy.
How long does it take for psoriatic arthritis treatments to work?
It varies. DMARDs like methotrexate can take 6-12 weeks. Biologics often show improvement in 4-8 weeks, with full effects at 3-6 months. Some newer oral drugs like deucravacitinib show results in as little as 4 weeks. Patience is key, but if there’s no change after 3 months, talk to your doctor about switching.
Can diet or supplements help?
No diet cures psoriatic arthritis. But some people find less inflammation with omega-3s (fish oil), vitamin D, and avoiding processed foods and alcohol. Weight loss can also reduce joint stress - especially in the knees. Supplements aren’t replacements for medication, but they can support overall health.
Is psoriatic arthritis hereditary?
Yes. If a close relative has psoriasis or psoriatic arthritis, your risk increases. Around 40% of people with the condition have a family history. Specific genes like HLA-B27 are linked to more severe forms, especially with spine involvement.
What to Do Next
If you’re experiencing joint pain along with skin or nail changes, don’t wait. Write down your symptoms: which joints hurt? When did it start? Do you have nail pitting? Has anyone in your family had psoriasis?
Bring that list to your doctor - preferably a rheumatologist or dermatologist who’s seen psoriatic arthritis before. Ask: “Could this be psoriatic arthritis?” Don’t accept a dismissal. Early treatment changes everything.
And if you’ve already been diagnosed - keep going. Even on meds, track your progress. Join a support group. Learn your triggers. Stay active. You’re not alone. And with the right care, you can live well - with strong joints, clear skin, and a full life ahead.







this literally saved my life. i had dactylitis for months and thought it was just injury from gym. turned out to be psoriatic arthritis. started on guselkumab and now i can hold my coffee without crying. thank you for writing this.
The biological link between cutaneous and articular inflammation is fascinating. The shared cytokine pathways-particularly IL-23/Th17-suggest a unified pathogenic mechanism rather than two coincident conditions. This has profound implications for targeted therapy development and early intervention strategies.
man i wish i read this 5 years ago. i was on methotrexate for ages, thought i was just getting old. then my derm said 'hey your nails look weird' and boom-psa. now i take a little pill instead of shots. life’s better. don’t wait like i did.
i had no idea my nail pitting was a clue. i thought it was just bad manicures. now i know why my knees felt like they were filled with cement every morning. this article made me cry. not from sadness-from relief. i’m not crazy. this is real. and it’s treatable.
There is a metaphysical dimension to autoimmune disease that science refuses to acknowledge. The body does not attack itself without a deeper signal-a disruption in the energetic harmony between mind and tissue. Psoriasis and arthritis are not random mutations; they are the physical manifestation of unresolved emotional stagnation. The immune system is not malfunctioning-it is screaming for integration. We treat the symptoms with biologics, yet ignore the soul’s cry for balance. Perhaps the real cure lies not in drugs, but in stillness, in surrender, in listening to what the body has been trying to tell us all along.
The notion that psoriatic arthritis is merely a manifestation of immune dysregulation is overly reductionist. One must consider the interplay of environmental triggers, epigenetic modulation, and psychosocial stressors that collectively prime the inflammatory cascade. The absence of a definitive biomarker does not negate the systemic nature of the condition; rather, it underscores the complexity of human immunobiology. It is imperative that clinical practice evolves beyond symptom suppression toward holistic restoration of homeostasis.
you are NOT alone. i was diagnosed 3 years ago and thought i was the only one who got that weird toe swelling. joined a support group and now i help new people every week. it’s hard but you can live full life. drink water, move slow, find your doc who listens. you got this 💪
why do we even bother with all this science? in america, you need insurance approval for a pill that costs more than your rent. my cousin took 18 months to get approved. meanwhile, his joints turned to dust. this isn’t medicine. it’s a lottery.
I find it curious that the article glorifies biologics as if they are panaceas. The pharmaceutical industry has a vested interest in chronicizing disease. What about the long-term immunosuppression risks? The rising incidence of lymphoma? The ecological cost of producing monoclonal antibodies? We are trading one problem for another, masked by marketing jargon and patient testimonials. A true solution requires systemic rethinking-not more pills.
I had psoriasis since i was 12 and never thought it would hit my joints. when my knuckles started locking up i went to a rheum and he said oh you probably have RA. i said no my skin is flaring right now. he looked at me like i was lying. took 3 months to get the right diagnosis. dont let them dismiss you. your skin knows what your joints are doing. trust it.
biologics are just a scam. my buddy took Humira for 2 years. got a fungal infection, then cancer. now he’s on chemo. this whole thing is a money grab. just eat turmeric and pray.
I understand the frustration with pharmaceutical profit motives, but dismissing biologics entirely ignores the lived reality of millions who regained mobility, function, and dignity because of them. The metaphysical framing you offered is poetic, but it doesn’t stop bone erosion. Science and soul aren’t mutually exclusive-they’re complementary. We need both the pill and the pause.