Thiazide & Vitamin D Safety Checker
Is Your Vitamin D Dose Safe With Thiazides?
Check if your vitamin D dose is within safe limits when taking thiazide diuretics. Many people take too much vitamin D, increasing their risk of dangerous hypercalcemia.
When you're taking a thiazide diuretic for high blood pressure and also popping a vitamin D supplement for bone health, you might think you're doing everything right. But there’s a quiet, dangerous overlap many people don’t know about - and it can push your blood calcium levels into dangerous territory.
Why This Combination Can Be Risky
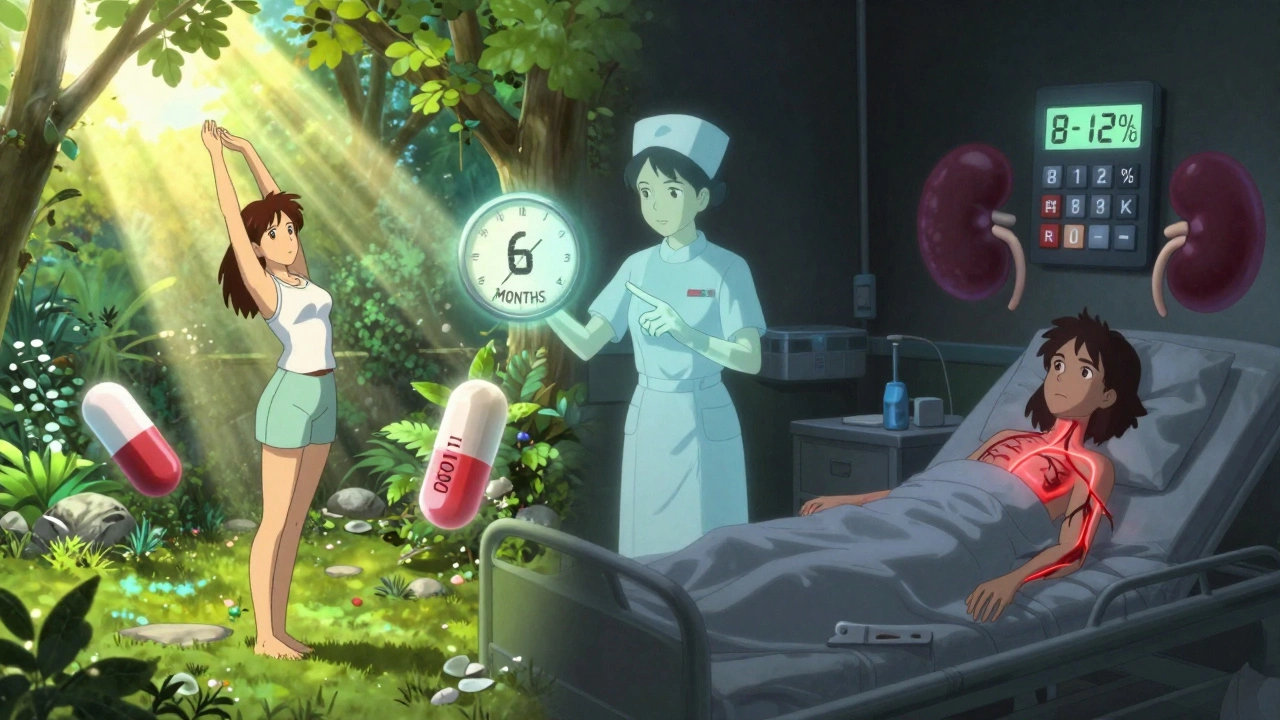
Thiazide diuretics like hydrochlorothiazide and chlorthalidone are common. They help lower blood pressure by making your kidneys get rid of extra salt and water. But here’s the twist: while they flush out sodium, they actually hold onto calcium. That’s not a bug - it’s how they work. By blocking a specific transporter in the kidney (the NCC channel), they cause your body to reabsorb more calcium than usual. This reduces urinary calcium loss by 30-40%. Meanwhile, vitamin D - especially in doses above 2,000 IU daily - ramps up how much calcium your gut absorbs from food. Its active form, calcitriol, turns on proteins like calbindin-D9k and TRPV6 that pull calcium into your bloodstream. Normally, this is helpful. But when you combine it with a thiazide, you’re essentially double-pumping calcium into your blood: one from your intestines, the other from your kidneys holding onto it. This isn’t theoretical. A 2021 study in the Journal of Clinical Endocrinology & Metabolism found that people taking high-dose vitamin D (over 4,000 IU/day) along with thiazides had an 8-12% chance of developing hypercalcemia. That’s more than triple the risk compared to those on thiazides alone. And in people over 65, nearly 22% of hypercalcemia cases traced back to this combo, according to Medicare data.What Is Hypercalcemia - And Why Should You Care?
Hypercalcemia means your blood calcium level is too high - usually above 10.5 mg/dL. At first, symptoms are vague: fatigue, nausea, constipation, frequent urination, or feeling unusually thirsty. Many people brush it off as aging, stress, or dehydration. But if left unchecked, calcium can deposit in your kidneys, leading to stones or even kidney damage. Severe cases can cause confusion, irregular heartbeat, or coma. The scary part? Most people don’t know they’re at risk. A 2022 survey by the National Council on Aging found that 61% of seniors on thiazides had no idea they needed to check their calcium levels when taking vitamin D. That’s not because they’re careless - it’s because the warning isn’t loud enough.Who’s Most at Risk?
You’re at higher risk if:- You’re over 65 - your kidneys don’t clear calcium as efficiently
- You’re taking more than 2,000 IU of vitamin D daily
- You have a history of kidney stones or kidney disease
- Your baseline calcium level is already above 10.2 mg/dL
- You’re taking multiple supplements, including calcium tablets
How Do Thiazides Compare to Other Diuretics?
Not all diuretics act the same. Loop diuretics like furosemide (Lasix) actually make your kidneys dump calcium - they’re the opposite of thiazides. If you’re on a loop diuretic and taking vitamin D, hypercalcemia isn’t a typical concern. Potassium-sparing diuretics like spironolactone don’t affect calcium reabsorption much either. So if you’re already on a thiazide and need vitamin D, switching to a potassium-sparing option might be safer - especially if you’re taking high-dose supplements. But here’s the catch: thiazides are still the top choice for hypertension in primary care. Why? They give better 24-hour blood pressure control than many alternatives, as shown in the SPRINT trial. So doctors keep prescribing them - even when patients are on vitamin D.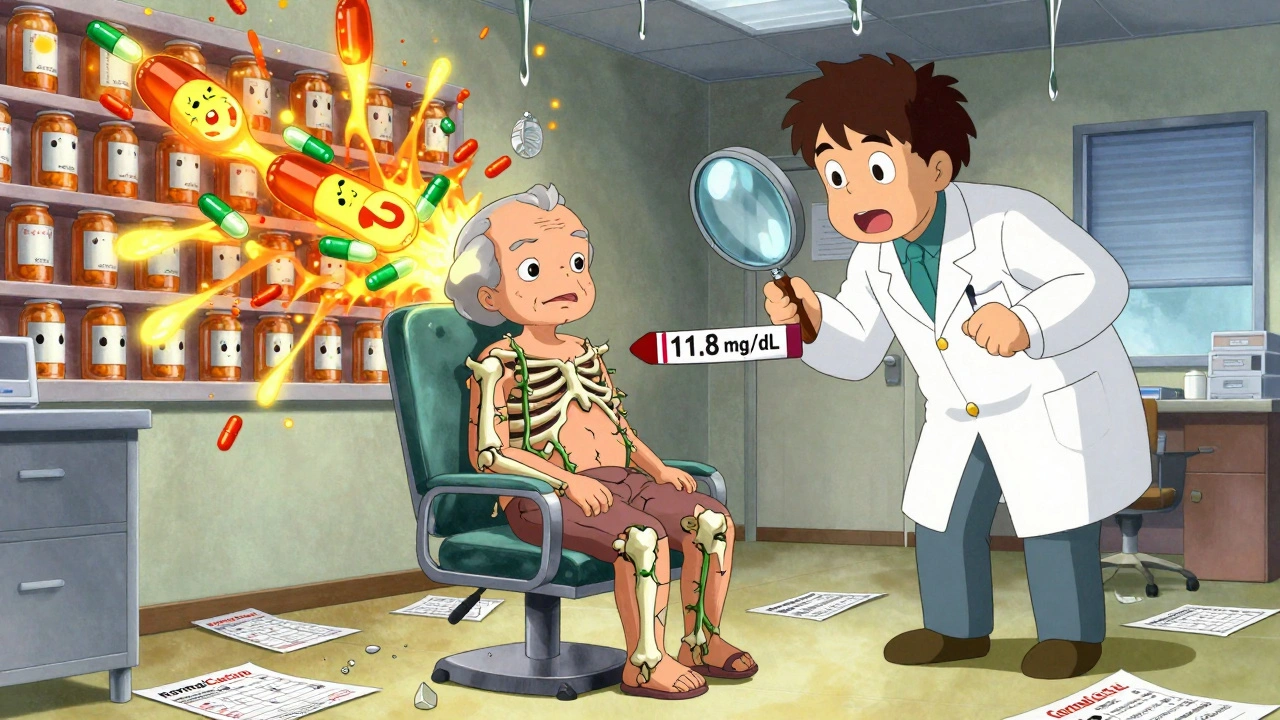
What Doses Are Safe?
There’s no one-size-fits-all answer, but guidelines give us a clear path:- Vitamin D: Stick to 800-1,000 IU daily if you’re on a thiazide. The Endocrine Society and European Society of Cardiology both recommend not exceeding 2,000 IU/day. Many people take 5,000 IU or more thinking “more is better,” but that’s where the danger kicks in.
- Thiazide dose: Use the lowest effective dose. Hydrochlorothiazide 12.5 mg works just as well for blood pressure as 25 mg - and carries less calcium-sparing risk.
- Calcium supplements: Avoid them unless you have a diagnosed deficiency. Most people get enough calcium from diet. Adding extra calcium on top of vitamin D and thiazides is like pouring gasoline on a fire.
Monitoring Is Non-Negotiable
If you’re on both, you need regular blood tests. Not once a year - every 3 to 6 months. The Kidney International Practice Guidelines are clear: baseline calcium before starting, then repeat every 3 months after beginning vitamin D, then every 6 months if stable. Your doctor should also check your corrected calcium - not just total calcium. Albumin levels affect the reading. If albumin is low (common in older adults or those with chronic illness), your total calcium might look normal when your free calcium is dangerously high. And yes - this is something your doctor should be tracking. But a 2023 American College of Physicians survey found that while 78% of internists knew about the interaction, only 42% knew the right monitoring schedule. If your doctor isn’t bringing it up, ask. Be specific: “Can we check my calcium levels every 6 months since I’m on HCTZ and vitamin D?”What Are the Alternatives?
If you’re worried, talk to your doctor about:- Switching diuretics: Spironolactone or amiloride don’t raise calcium levels. They’re not first-line for hypertension, but they’re safer with vitamin D.
- Lowering vitamin D: Go from 5,000 IU to 1,000 IU. Most people don’t need more than that, even if they’ve been told otherwise.
- Trying a newer thiazide-like drug: Metolazone may have a weaker effect on calcium reabsorption (only 25% reduction vs. 35-42% for traditional thiazides), based on research presented at the 2023 American Society of Nephrology meeting.
- Getting sunlight: If you’re taking vitamin D for deficiency, try 10-15 minutes of midday sun a few times a week. Your body makes vitamin D naturally without the risk of overdose.
What’s Changing in 2025?
This isn’t a static issue. In 2023, the FDA approved a new genetic test called CalcCheck that looks at your calcium-sensing receptor gene. It can predict whether you’re genetically more likely to develop hypercalcemia on this combo. It’s not widely available yet, but it’s coming. Kaiser Permanente already uses EHR alerts that pop up when a patient is prescribed vitamin D over 2,000 IU while on a thiazide. Since implementing this, they’ve cut unsafe combinations by 63%. The American Heart Association’s new guidelines, expected in early 2025, will likely tighten recommendations even further. They’re already warning that this interaction is one of the most underrecognized causes of drug-induced hypercalcemia in older adults.Real Stories, Real Consequences
On Drugs.com, 32% of negative reviews for hydrochlorothiazide mention calcium-related side effects. One patient wrote: “I took 5,000 IU of D3 for years with my HCTZ. I got so tired I couldn’t work. My calcium was 11.8. I ended up in the ER. No one ever told me this could happen.” But not all stories are bad. A 2022 CureTogether report found that 45% of patients on low-dose vitamin D (800-1,000 IU) with thiazides had normal calcium levels - and even saw a 1.8% annual improvement in bone density. That’s the sweet spot: enough vitamin D to protect bones, not enough to overload your system.What You Can Do Today
1. Check your supplement bottle. If it says 5,000 IU or more, talk to your doctor about lowering it. 2. Ask for a recent calcium blood test. If you haven’t had one in over a year, request it. 3. Don’t take calcium pills unless prescribed. Food and sunlight are safer sources. 4. Know your numbers. Normal calcium is 8.6-10.2 mg/dL. Above 10.5 is high. Above 11 is dangerous. 5. Speak up. If your doctor doesn’t mention this interaction, bring it up. You’re not being difficult - you’re protecting your health. This isn’t about avoiding medication. Thiazides save lives. Vitamin D helps bones. But together, without awareness, they can create a silent storm. The solution isn’t to stop - it’s to be smart about how you take them.Can vitamin D and thiazide diuretics cause high calcium levels?
Yes. Thiazide diuretics reduce calcium loss in urine, while vitamin D increases calcium absorption from food. Together, they can push blood calcium levels into the dangerous range (hypercalcemia), especially with doses above 2,000 IU of vitamin D daily. Studies show this combination increases hypercalcemia risk to 8-12% in people taking high-dose supplements.
What vitamin D dose is safe with thiazide diuretics?
Stick to 800-1,000 IU per day. The Endocrine Society and European Society of Cardiology recommend not exceeding 2,000 IU daily when on thiazides. Most people don’t need more than this, even if they’ve been told to take higher doses for bone health. High-dose supplements (5,000 IU or more) significantly raise the risk of hypercalcemia.
How often should calcium levels be checked when taking both?
Check calcium levels before starting vitamin D, then every 3 months after beginning supplementation. If levels stay normal, continue testing every 6 months. Annual checks aren’t enough - this interaction can develop quickly, especially in older adults or those with kidney changes.
Are there safer diuretics to use with vitamin D?
Yes. Potassium-sparing diuretics like spironolactone and amiloride don’t reduce calcium excretion, so they’re safer when combined with vitamin D. Loop diuretics like furosemide actually increase calcium loss, making them a lower-risk option too. However, thiazides are still preferred for blood pressure control in many cases, so switching should be discussed with your doctor.
What are the symptoms of hypercalcemia from this interaction?
Early symptoms include fatigue, nausea, constipation, increased thirst, and frequent urination. Later signs may involve confusion, muscle weakness, irregular heartbeat, or kidney stones. Many people mistake these for normal aging or stress, which delays diagnosis. If you’re on thiazides and vitamin D and feel unusually tired or constipated, ask for a calcium blood test.
Should I stop taking vitamin D if I’m on a thiazide?
No - but do lower the dose. Most people don’t need more than 800-1,000 IU daily, even with thiazides. Stopping vitamin D entirely can harm bone health. The goal is balance: enough to support bones, not enough to overload your system. Monitor your calcium levels and work with your doctor to find the safest dose for you.









Too much D3 with HCTZ? Yeah, I knew someone who got hospitalized for this.
People just pop supplements like candy. No lab work, no doctor talk. You think vitamin D is harmless? It's a hormone, not a vitamin. And thiazides? They're not harmless either. You combine them without monitoring? That's not health-it's negligence. And now you're surprised you feel like garbage? You're not special. You're just unlucky.
I've been on HCTZ for 8 years and took 2000 IU of D3 for a while. Didn't think twice until I started feeling like I'd been dragged through a swamp-constant fatigue, weird constipation, always thirsty. Got my calcium checked last year-10.7. My PCP just shrugged and said, 'Eh, it's fine.' I had to push. Now I'm down to 800 IU, and I feel like I got my energy back. I wish someone had told me this sooner. Not everyone's got the energy to fight for their own health.
THE FDA KNOWS. THEY'VE KNOWN FOR YEARS. WHY ISN'T THIS ON THE LABEL?!?!!?!!? THE PHARMA COMPANIES ARE HIDING THIS. THEY DON'T WANT YOU TO KNOW THAT YOUR 'BONE HEALTH' SUPPLEMENT IS ACTUALLY A TIME BOMB WHEN MIXED WITH YOUR BP MED. THEY MAKE BILLIONS OFF THIS. THEY DON'T CARE IF YOU GET KIDNEY STONES OR FALL INTO A COMA. THIS IS A COVER-UP. ASK YOURSELF-WHY DOESN'T THE FDA FORCE WARNINGS? BECAUSE THEY'RE IN BED WITH BIG PHARMA. YOU THINK YOU'RE BEING HEALTHY? YOU'RE BEING USED.
so like… if you on hctz and take vit d… you gotta check your calcium? i had no idea. i been taking 5000iu for years. i thought more is better. my doctor never said nothin. now im scared. maybe i should go get it checked. i been kinda tired lately…
I just want to say-this is such an important post. So many of us are just trying to do the right thing: take our meds, take our vitamins, stay healthy. But we’re not given the full picture. I’m so glad you laid this out so clearly. I’ve been telling my mom to cut her D3 down from 5000 to 1000 since she’s on HCTZ, and she finally listened after reading this. She’s been feeling better already. You’re not just sharing info-you’re saving lives. Thank you.
How quaint. A 2021 study? How pedestrian. The real issue is the abysmal state of American medical education-where general practitioners are trained to prescribe like automatons and never to question the synergy of pharmacological cascades. The vitamin D-thiazide interaction is not merely a risk-it’s a symphony of iatrogenic folly, orchestrated by corporate guidelines and the collective laziness of clinical oversight. One wonders if the FDA even knows what calcitriol is anymore.
MY DAD WAS IN THE ER LAST YEAR BECAUSE OF THIS!! HE TOOK 5000 IU OF D3 AND HCTZ FOR 3 YEARS AND NO ONE TOLD HIM!! HE GOT CONFUSED, COULDN’T WALK, HAD TO BE HOSPITALIZED FOR 5 DAYS!! I’M SO ANGRY!! WHY ISN’T THIS A BIGGER STORY?! WHY AREN’T PHARMACISTS ALERTING PEOPLE?! THIS IS A TRAGEDY WAITING TO HAPPEN TO EVERYONE!!
life’s weird, right? we take pills to feel better, but sometimes the pills we think are helping are quietly messing with us. i used to take 5k IU of D3 with my hctz. felt fine. then i started sleeping 12 hours and still tired. got my levels checked-calcium was 10.9. switched to 1k IU. within two weeks, i felt like i could breathe again. no magic, just biology. we’re not machines. our bodies notice when we overload them. sometimes, less really is more. 🌿
Why are we letting foreigners tell us how to take our medicine? In America, we know what’s best. Vitamin D? We need it. Thiazides? We need them. If you can’t handle it, maybe you shouldn’t be on meds. Stop being so weak. This is just another liberal panic over supplements. We’ve been taking this combo for decades. People are fine. Let’s focus on real problems.
From a pharmacokinetic standpoint, the NCC transporter inhibition by thiazides creates a physiologic calcium-sparing effect that synergizes with calcitriol-mediated upregulation of TRPV6 and calbindin-D9k in enterocytes. This results in a net increase in serum ionized calcium above the renal threshold for reabsorption. The clinical risk is amplified in elderly patients due to age-related decline in GFR and reduced albumin synthesis, which skews corrected calcium values. Monitoring should include both total and ionized calcium, with albumin-adjusted calculations. Most primary care providers lack training in this nuance. The 3-6 month monitoring window is evidence-based but underutilized.
lol i just take my pills and hope for the best 😅