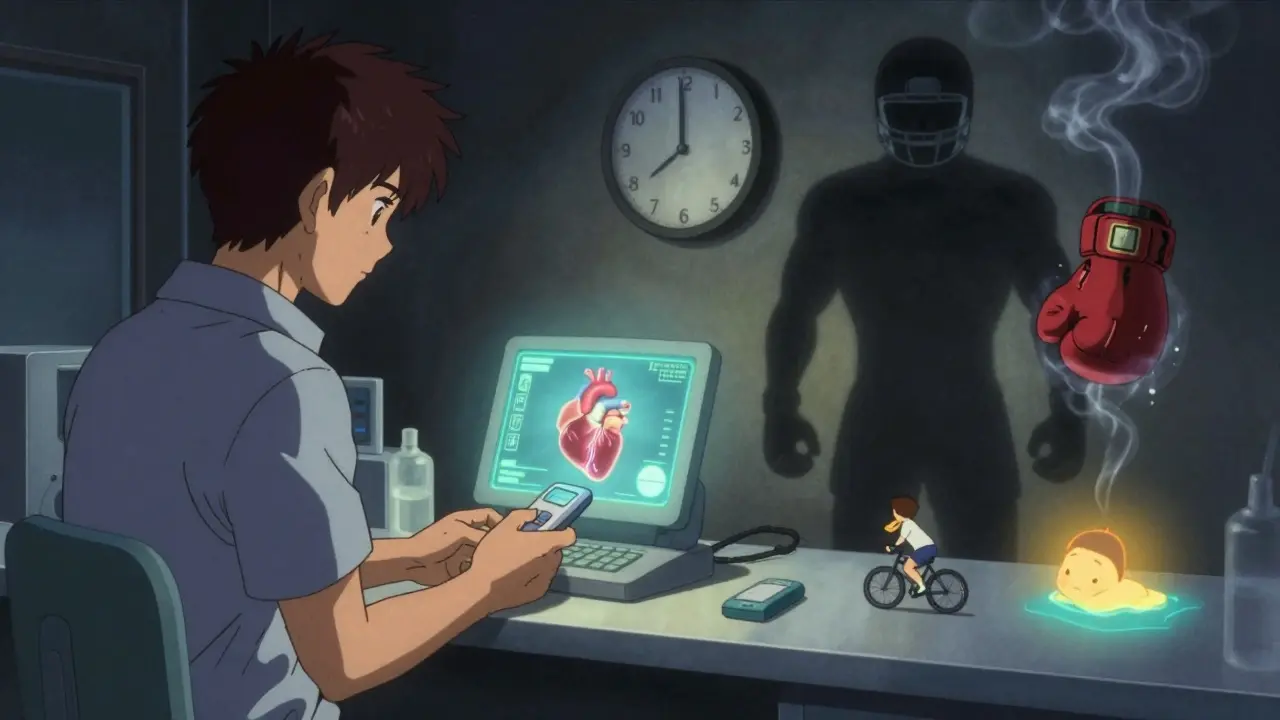
Anticoagulant Sports Risk Calculator
Calculate Your Sports Injury Risk
Select your medication type and sport category to see your relative bleeding risk and personalized recommendations.
Your Risk Assessment
Medium RiskHigh-risk sports with warfarin carry significant bleeding danger due to unpredictable effects and need for frequent monitoring.
Key Considerations:
- Warfarin has a higher risk of bleeding with high-impact sports compared to DOACs
- DOACs like apixaban have shorter half-lives, making them safer for athletic activities when timed properly
- Protective gear can reduce risk by 76% in low-impact sports
Playing sports while on blood thinners isn’t just risky-it’s a calculated decision that can make the difference between staying active and facing a life-threatening bleed. Athletes with conditions like atrial fibrillation or a history of blood clots are increasingly turning to anticoagulants to protect their hearts and veins. But when you’re sprinting, tackling, or crashing on a bike, the same drugs that prevent clots can turn a minor fall into a medical emergency.
Why Athletes on Blood Thinners Face Higher Bleeding Risks
Normal people might bruise easily on blood thinners. Athletes? They’re at risk of internal bleeding from impacts most of us never feel. Studies show athletes on anticoagulants are 3 to 5 times more likely to suffer major bleeding during sports than non-athletes. Why? Because sports aren’t just physical-they’re violent by design.
In American football, a single tackle can generate over 5G of force. Ice hockey checks, rugby scrums, even a hard slide in soccer-these aren’t accidents. They’re part of the game. And when your blood doesn’t clot the way it should, those forces don’t just hurt-they bleed.
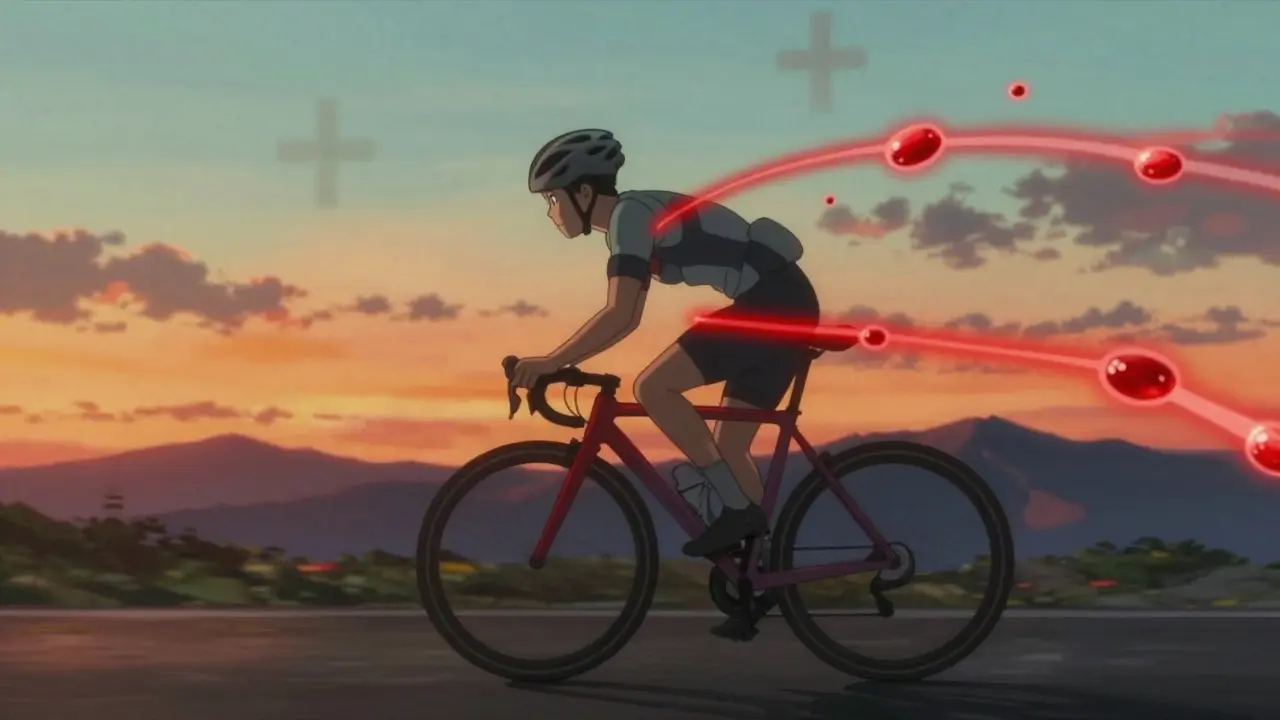
One study tracking anticoagulated athletes found a 22.7% major bleeding rate in high-contact sports like boxing or rugby. In low-impact activities like swimming or cycling? Just 1.3%. That’s not a small gap. It’s a chasm.
The Three Categories of Sports Risk
Not all sports are created equal when you’re on blood thinners. Experts classify them into three clear tiers based on trauma risk:
- High-risk sports: Football, hockey, boxing, rugby, wrestling. These involve direct, high-force collisions. Participation is strongly discouraged by the American Heart Association and European Society of Cardiology. Even one impact can trigger a fatal bleed.
- Intermediate-risk sports: Basketball, soccer, skiing, lacrosse. These have frequent contact, but not constant. Shared decision-making is required. Some athletes continue with strict precautions, but the risk is real.
- Low-risk sports: Running, cycling, swimming, rowing, yoga. Minimal trauma, predictable movements. These are generally safe with proper management.
The difference isn’t just about contact. It’s about force, frequency, and unpredictability. A fall on a bike might be avoidable. A blindside hit in basketball? Not so much.
Warfarin vs. DOACs: Which Is Safer for Athletes?
Not all blood thinners are the same. Two main types are used: warfarin and direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran.
Warfarin has been around for decades. It works by blocking vitamin K, but it’s finicky. Your INR (a blood test measuring clotting time) must stay between 2.0 and 3.0. Too low? Clots form. Too high? You bleed. And it’s affected by diet, alcohol, other meds-even a change in your sleep schedule can throw it off. Weekly blood tests are common. That’s not practical for athletes training 6 days a week.
DOACs are newer. They’re more predictable. No weekly INR checks. Fewer food interactions. Their half-lives are short: apixaban clears in 8-15 hours, rivaroxaban in 5-13. That’s a game-changer.
Here’s the kicker: a 2025 JAMA study of over 160,000 patients showed apixaban had the lowest risk of both recurring clots and major bleeding compared to rivaroxaban and warfarin. For athletes, that’s the gold standard.
But there’s a catch. DOACs aren’t safe for everyone. If you have a mechanical heart valve, DOACs are strictly forbidden. Warfarin is still the only option there.

Four Proven Strategies to Stay Active Safely
Can you still compete? Yes-but only with a smart, personalized plan. Here are four strategies backed by clinical evidence:
- Switch to low-impact sports: Runners and cyclists who wear helmets, pads, and avoid crowded trails reduce their bleeding risk from 8.2% to just 1.9%. Protective gear isn’t optional-it’s essential.
- Temporarily lower your warfarin dose: Some athletes reduce warfarin 3-4 days before a game to bring INR down to 1.5-1.8. It’s risky. Recurrent clot risk jumps to 0.8% per event. Only consider this with close monitoring and never for high-risk sports.
- Use LMWH with timed breaks: Enoxaparin (a daily injection) can be stopped 24 hours before competition. It clears fast, keeps clot protection strong, and cuts bleeding risk by 42%. This works well for athletes with short, intense seasons.
- Time your DOAC dose: This is the most promising approach. Since apixaban’s effect drops sharply after 20-24 hours, taking your dose 24 hours before competition leaves you with minimal anticoagulation during the event. One professional cyclist did this for two seasons with zero clots or bleeds. But it requires special blood tests-anti-Xa assays-to confirm levels are safe.
None of these are one-size-fits-all. The right choice depends on your condition, sport, and personal risk tolerance.
What the Experts Say
Dr. Paul D. Thompson, who helped write the AHA/ACC guidelines, puts it bluntly: “You’re not just treating a clot. You’re managing an athlete’s life.”
Dr. Matteo Palamà, lead author of a 2023 review in the European Heart Journal, says DOACs are now the first choice for athletes because their short half-life lets you “turn off” the effect without triggering dangerous rebound clotting.
But here’s the problem: almost no clinical trials include athletes. Only 0.3% of participants in major anticoagulant studies were competitive athletes. That means most guidelines are based on data from sedentary patients. We’re guessing-based on experience, not hard evidence.
How Sports Organizations Are Responding
Professional leagues aren’t ignoring this. The NBA requires players on warfarin to have an INR below 2.0 to play. The UCI, which governs cycling, allows DOACs but demands a 24-hour pre-event dose pause. These aren’t suggestions-they’re rules.
And the numbers show change is happening. In 2015, only 32% of athletic trainers consulted formal anticoagulation guidelines before clearing athletes. By 2022, that number jumped to 78%. More teams now have cardiologists on call for these cases.
And good news: the World Anti-Doping Agency confirmed in 2020 that therapeutic anticoagulants don’t count as doping-as long as you have proper documentation. No need to hide your meds.
The Future: Precision Medicine for Athletes
The next frontier? Personalized dosing. A 2023 NIH study used pharmacokinetic modeling to predict the perfect dosing window for each athlete. The result? 92% of participants found a safe schedule. Two-thirds were able to keep competing.
Tools like the CoaguChek INRange device-FDA-cleared in March 2023-let athletes test their INR at home with 95% accuracy. No more driving to a lab after a late-night workout.
And research is getting even smarter. Wearable sensors are now measuring impact forces in real time during sports. In pilot studies, researchers are mapping how hard a soccer tackle hits, how fast a skier crashes, how much force a rugby scrum generates. This data will soon feed into algorithms that tell you: “Based on your sport, your drug, and your body, you can safely compete if your dose is taken at 8 p.m. the night before.”
By 2028, the American College of Sports Medicine predicts a 40% rise in athlete anticoagulation consultations. As more athletes live longer with heart conditions, this won’t be a niche issue. It’ll be standard care.
What You Need to Do Right Now
If you’re on blood thinners and want to play sports:
- Know your exact diagnosis. Is it atrial fibrillation? A past clot? A mechanical valve?
- Know your drug. Warfarin? Apixaban? Something else?
- Know your sport’s risk level. High, medium, or low?
- Work with a cardiologist who understands sports medicine-not just a generalist.
- Never skip blood tests. Even if you feel fine, your INR or anti-Xa level might not be.
- Wear protective gear. Always. Even in low-risk sports.
There’s no magic pill that lets you play football safely on anticoagulants. But with the right plan, you can still run, swim, bike, and compete-at the level you love-without putting your life on the line.
Can I still play basketball if I’m on a blood thinner?
Basketball is classified as an intermediate-risk sport due to frequent contact and sudden impacts. While not outright prohibited, it carries a significant bleeding risk for those on anticoagulants. Most experts recommend avoiding it unless you’ve switched to a DOAC like apixaban and can implement a timed dosing strategy-taking your dose 24 hours before games to reduce anticoagulant levels during play. Even then, protective gear, close monitoring, and a cardiologist’s clearance are mandatory. Many athletes in this situation choose to switch to lower-risk activities like swimming or cycling.
Is warfarin ever safe for athletes?
Warfarin is rarely ideal for athletes because of its unpredictable effects and need for frequent INR monitoring. It’s only recommended for those with mechanical heart valves, where DOACs are strictly contraindicated. Even then, athletes on warfarin must avoid high-impact sports and may need to reduce their dose before competitions, which increases clot risk. For most athletes, switching to a DOAC like apixaban is a safer and more practical option.
Can I take my blood thinner on the day of a race?
It depends on the drug. For DOACs like apixaban or rivaroxaban, taking your dose 24 hours before the event is a proven strategy to lower bleeding risk while maintaining protection. For warfarin, skipping doses is risky and can trigger clots. For LMWH injections, the dose is usually skipped 24 hours before competition. Never adjust your dose without consulting your doctor and running a blood test to confirm your levels are safe.
Do I need to tell my coach or team about my blood thinner?
Yes. Your coach, trainer, and teammates should know you’re on anticoagulants. In case of a fall or injury, they need to recognize the signs of internal bleeding-unusual swelling, extreme fatigue, dizziness, or pain-and act immediately. Many teams now include anticoagulation status in emergency medical profiles. It’s not just about safety-it’s about preparedness.
Are there any sports I should never play on blood thinners?
Yes. High-contact sports like boxing, football, hockey, rugby, and wrestling are strongly discouraged-and often banned by medical guidelines-for anyone on therapeutic anticoagulation. The force of impact in these sports is too unpredictable and too high. Even a single collision can cause a life-threatening bleed. No amount of protective gear can fully offset this risk. These sports should be avoided entirely.
Final Thought: It’s Not About Giving Up-It’s About Playing Smarter
Being on blood thinners doesn’t mean you have to hang up your cleats or quit your sport. It means you have to be smarter. It means listening to your body, tracking your numbers, and working with the right team of doctors. The goal isn’t to eliminate risk-it’s to manage it. And with today’s tools, that’s not just possible. It’s doable.






Let me get this straight-you’re telling me some dude on apixaban is gonna lace up for a pickup game of basketball like it’s just another Tuesday? That’s not bravery, that’s clinical negligence. We’re talking about a drug that turns a stumble into a hemorrhage. The AHA doesn’t mince words: intermediate-risk sports are a gamble with your life. And you think a 24-hour dose delay is some kind of hack? Please. You’re not managing risk-you’re playing Russian roulette with your internal organs. If your cardiologist signed off on this, they’re either incompetent or on the take.
Frankly, the entire discourse is predicated on a flawed epistemological framework-relying on observational cohort data from sedentary populations to inform athletic decision-making is a category error of the highest order. The pharmacokinetic modeling referenced is promising, yes, but without RCTs in high-performance cohorts, we’re essentially engineering a safety protocol on the back of a cocktail napkin. DOACs may have lower bleeding incidence, but the absence of trauma-specific biomarkers in current guidelines renders any ‘safe’ dosing window purely speculative. We need longitudinal, sport-specific pharmacodynamic mapping. Until then, this is all narrative medicine dressed in algorithmic clothing.
Man, I used to play kabaddi back home in Kerala-tackles, dives, the whole shebang. My uncle was on warfarin after a stroke, and he’d still go out with his buddies, just swapped the hard hits for slow, controlled moves. Said it kept his mind sharp as much as his blood thin. Maybe it ain’t about giving up the game, but changing the rhythm of it. You don’t have to be the guy who crashes through the line-you can be the one who reads the play, slips away, stays alive. Different kind of strength, y’know?
bro why are you even on blood thinners if you wanna play sports like a maniac?? like if you got afib just sit on the couch and watch nba. why risk it? i had a cousin who did a 360 spin on a bike and cracked his skull and bled out in 10 mins cause he was on rivaroxaban. dont be stupid. just dont. its not worth it.
Let’s be real-this whole ‘DOACs are safer’ narrative is corporate propaganda masquerading as science. Apixaban’s half-life? Sure, it’s shorter. But what about the rebound hypercoagulable state after 24 hours? No one talks about that. And who’s monitoring the anti-Xa levels? The average athlete isn’t running lab tests before every game. And don’t even get me started on the fact that 97% of the data comes from people who don’t even know what a plyometric jump is. We’re applying cardiac guidelines to athletes like they’re 70-year-olds with pacemakers. This isn’t medicine. It’s institutional cowardice wrapped in a white coat.
There’s a deeper truth here, and it’s not in the INR values or the half-lives-it’s in the myth of control. We think we can quantify risk, time doses, wear pads, and outsmart biology. But the body doesn’t care about your spreadsheet. It doesn’t care that you took your apixaban at 8 p.m. The moment your shoulder hits the floor during a layup, physics takes over. And physics? Physics doesn’t negotiate. This isn’t about sports or drugs-it’s about the human delusion that we can bend mortality to our will. We’re not athletes on anticoagulants. We’re mortals playing dress-up in cleats, pretending the reaper doesn’t have a stopwatch.
Oh wow, so now we’re giving athletes a ‘timed dosing strategy’ like they’re rocket scientists launching a satellite? Next they’ll be prescribing pre-game smoothies with vitamin K antagonists and a side of panic. And let’s not forget the UCI’s ‘rule’-because nothing says ‘sports integrity’ like a bureaucrat deciding when your blood can clot. Meanwhile, the guy who plays pickup basketball with a broken wrist and three beers in him? He’s fine. But you? You’re a liability. Congrats. You’re now the most regulated person in the gym.
Hey everyone-just wanted to say thank you for this thread. I’m a runner with AFib on apixaban, and I used to feel so alone in this. I switched from basketball after a scary fall last year, and now I do trail running with a medical alert bracelet and a phone on my arm. My coach knows, my running group knows, and I check my INR every 6 weeks with my home device. It’s not the life I planned, but it’s the life I get to keep. You don’t have to quit your passion-you just have to redefine it. And that’s okay. You’re still an athlete. Just a smarter one.
Let’s be honest-this whole article reads like a pharmaceutical white paper disguised as medical advice. DOACs are expensive. Warfarin is cheap. Who benefits from pushing apixaban as the ‘gold standard’? The 2025 JAMA study? That’s a reanalysis of post-hoc data with selection bias thicker than a linebacker’s neck. And don’t even get me started on the ‘wearable impact sensors’-next thing you know, we’ll have AI telling you your tackle was 4.8G and your dose was 0.2mg too high. This isn’t progress. It’s monetized fear.